Abstract
Human transmissible spongiform encephalopathies (TSEs), or prion diseases, are invariably fatal conditions associated with a range of clinical presentations. TSEs are classified as sporadic [e.g. sporadic Creutzfeldt–Jakob disease (sCJD), which is the most frequent form], genetic (e.g. Gerstmann–Straussler–Scheinker disease, fatal familial insomnia, and inherited CJD), and acquired or infectious (e.g. Kuru, iatrogenic CJD, and variant CJD). In the past, brain imaging played a supporting role in the diagnosis of TSEs, whereas nowadays magnetic resonance imaging (MRI) plays such a prominent role that MRI findings have been included in the diagnostic criteria for sCJD. Currently, MRI is required for all patients with a clinical suspicion of TSEs. Thus, MRI semeiotics of TSEs should become part of the cultural baggage of any radiologist. The purposes of this update on the neuroradiology of CJD are to (i) review the pathophysiology and clinical presentation of TSEs, (ii) describe both typical and atypical MRI findings of CJD, and (iii) illustrate diseases mimicking CJD, underlining the MRI key findings useful in the differential diagnosis.















Similar content being viewed by others
References
Heiseke A, Aguib Y, Riemer C, Baier M, Schatzl HM (2009) Lithium induces clearance of protease resistant prion protein in prion-infected cells by induction of autophagy. J Neurochem 109:25–34
Sim VL, Caughey B (2009) Recent advances in prion chemotherapeutics. Infect Disord Drug Targets 9:81–91
Panegyres PK, Armari E (2013) Therapies for human prion diseases. Am J Neurodegener Dis 2(3):176–186
Zou WQ, Puoti G, Xiao X, Yuan J, Qing L, Cali I et al (2010) Variably protease-sensitive prionopathy: a new sporadic disease of the prion protein. Ann Neurol 68:162–172
Rinne ML, McGinnis SM, Samuels MA, Katz JT, Loscalzo J (2012) Clinical problem-solving. A startling decline. N Engl J Med 366(9):836–842
Moreno JA, Radford H, Peretti D, Steinert JR, Verity N, Guerra Martin MG et al (2012) Sustained translational repression by elF2α-P mediates prion neurodegeneration. Nature 485:507–511
Macfarlane RG, Wroe SJ, Collinge J, Yousry TA, Jager HR (2007) Neuroimaging findings in human prion disease. J Neurol Neurosurg Psychiatry 78:664–670
Vitali P, Maccagnano E, Caverzasi E, Henry RG, Haman A, Torres-Chae C et al (2011) Diffusion-weighted MRI hyperintensity patterns differentiate CJD from other rapid dementias. Neurology 76:1711–1719
Newey CR, Sarwal A, Wisco D, Alam S, Lederman RJ (2013) Variability in diagnosing Creutzfeldt–Jakob disease using standard and proposed diagnostic criteria. J Neuroimaging 23(1):58–63
Gibbons RV, Holman RC, Belay ED, Schonberger LB (2000) Creutzfeldt–Jakob disease in the United States: 1979–1998. JAMA 284(18):2322–2323
Klug GM, Boyd A, Lewis V, Douglass SL, Argent R, Lee JS, Australian National Creutzfeldt–Jakob Disease Registry et al (2006) Creutzfeldt–Jakob disease: Australian surveillance update to December 2005. Commun Dis Intell Q Rep 30(1):144–147
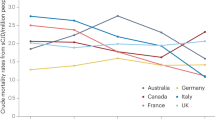
Ladogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S et al (2005) Mortality from Creutzfeldt–Jakob disease and related disorders in Europe, Australia, and Canada. Neurology 64(9):586–591
Appleby BS, Appleby KK, Crain BJ, Onyike CU, Wallin MT, Rabins PV (2009) Characteristics of established and proposed sporadic Creutzfeldt–Jacob disease variants. Arch Neurol 66(2):208–215
Del Barrio-Manso I, Toribio-García A, Cordero-Coma M, Tuñón L, Baragaño E (2010) Creutzfeldt–Jakob presenting with isolated visual symptoms: the Heidenhain variant. Arch Soc Esp Oftalmo 85(10):341–344
Meissner B, Kallenger K, Sanchez-Juan P, Collie D, Summers DM, Almonti S et al (2009) MRI lesions profiles in sporadic Creutzfeldt–Jacob disease. Neurology 72:1994–2001
Parchi P, de Boni L, Saverioni D, Cohen ML, Ferrer I, Gambetti P et al (2012) Consensus classification of human prion disease histotypes allows reliable identification of molecular subtypes: an inter-rater study among surveillance centres in Europe and USA. Acta Neuropathol 124(4):517–529
Wadsworth JD, Collinge J (2011) Molecular pathology of human prion disease. Acta Neuropathol 121:69–77
Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Heinemann U et al (2009) Updated clinical diagnostic criteria for sporadic Creutzfeldt–Jakob disease. Brain 132:2659–2668
Chohan G, Pennington C, Mackenzie JM, Andrews M, Everington D, Will RG et al (2010) The role of cerebrospinal fluid 14-3-3 and other proteins in the diagnosis of sporadic Creutzfeldt–Jakob disease in the UK: a 10-year review. J Neurol Neurosurg Psychiatry 81:1243–1248
Muayqil T, Gronseth G, Camicioli R (2012) Evidence-based guideline: diagnostic accuracy of CSF 14-3-3 protein in sporadic Creutzfeldt–Jakob disease: report of the guideline development subcommittee of the American Academy of Neurology. Neurology 79(14):1499–1506
Orrù CD, Wilham JM, Vascellari S, Hughson AG, Caughey B (2012) New generation QuIC assays for prion seeding activity. Prion 6(2):147–52
Zanusso G, Monaco S, Pocchiari M, Caughey B (2016) Advanced tests for early and accurate diagnosis of Creutzfeldt–Jakob disease. Nat Rev Neurol 12(6):325–333
Luk C, Jones S, Thomas C, Fox NC, Mok TH, Mead S et al (2016) Diagnosing sporadic Creutzfeldt–Jakob disease by the detection of abnormal prion protein in patient urine. JAMA Neurol 73(12):1454–1460
Sharma S, Mukherjee M, Kedage V, Muttigi MS, Rao A, Rao S (2009) Sporadic Creutzfeldt–Jacob disease—a review. Int J Neurosci 119:1981–1994
Kovács GG, Puopolo M, Ladogana A, Pocchiari M, Budka H, van Duijn C, EUROCJD et al (2005) Genetic prion disease: the EUROCJD experience. Hum Genet 118(2):166–174
Brown P, Preece M, Brandel JP, Sato T, McShane L, Zerr I et al (2000) Iatrogenic Creutzfeldt–Jakob disease at the millennium. Neurology 55(8):1075–1081
Lee J, Kim SY, Hwang KJ, Ju YR, Woo HJ (2013) Prion diseases as transmissible zoonotic diseases. Osong Public Health Res Perspect 4(1):57–66
Brandel JP, Peckeu L, Haïk S (2013) The French surveillance network of Creutzfeldt–Jakob disease. Epidemiological data in France and worldwide. Transfus Clin Biol 20(4):395–397
Hill AF, Butterworth RJ, Joiner S, Jackson G, Rossor MN, Thomas DJ et al (1999) Investigation of variant Creutzfeldt–Jakob disease and other human prion diseases with tonsil biopsy samples. Lancet 353(9148):183–189
García Santos JM, López Corbalán JA, Martínez-Lage JF, Sicilia Guillén J (1996) CT and MRI in iatrogenic and sporadic Creutzfeldt–Jakob disease: as far as imaging perceives. Neuroradiology 38(3):226–231
Kallenberg K, Schulz-Schaeffer WJ, Jastrow U, Poser S, Meissner B, Tschampa HJ et al (2006) Creutzfeldt–Jakob disease: comparative analysis of MR imaging sequences. AJNR Am J Neuroradiol 27:1459–1462
Lodi R, Parchi P, Tonon C, Manners D, Capellari S, Strammiello R et al (2009) Magnetic resonance diagnostic markers in clinically sporadic prion disease: a combined brain magnetic resonance imaging and spectroscopy study. Brain 132(10):2669–2679
Figini M, Alexander DC, Redaelli V, Fasano F, Grisoli M, Baselli G et al (2015) Mathematical models for the diffusion magnetic resonance signal abnormality in patients with prion diseases. Neuroimage Clin 7:142–154
Lee H, Hoffman C, Kingsley PB, Degnan A, Cohen O, Prohovnik I (2010) Enhanced detection of diffusion reductions in Creutzfeldt–Jakob disease at a higher B factor. AJNR Am J Neuroradiol 31(1):49–54
Hyare H, Thornton J, Stevens J, Mead S, Rudge P, Collinge J et al (2010) High-b-value diffusion MR imaging and basal nuclei apparent diffusion coefficient measurements in variant and sporadic Creutzfeldt–Jakob disease. AJNR Am J Neuroradiol 31(3):521–526
Puoti G, Bizzi A, Forloni G, Safar JG, Tagliavini F, Gambetti P (2012) Sporadic human prion diseases: molecular insights and diagnosis. Lancet Neurol 11(7):618–28
Kong A, Kleinig T, Van der Vliet A, Bergin P, Coscia C, Ring S et al (2008) MRI of sporadic Creutzfeldt–Jacob disease. J Med Imaging Radiat Oncol 52:318–324
Lee H, Cohen OS, Rosenmann H, Hoffmann C, Kingsley PB, Korczyn AD et al (2012) Cerebral white matter disruption in Creutzfeldt–Jakob disease. AJNR Am J Neuroradiol 33(10):1945–1950
Galanaud D, Haik S, Linguraru MG, Ranjeva JP, Faucheux B, Kaphan E et al (2010) Combined diffusion imaging and MR spectroscopy in the diagnosis of human prion diseases. AJNR Am J Neuroradiol 31(7):1311–1318
Kim JH, Choi BS, Jung C, Chang Y, Kim S (2011) Diffusion-weighted imaging and magnetic resonance spectroscopy of sporadic Creutzfeldt Jacob disease: correlation with clinical course. Neuroradiology 53(12):939–945
Clarencon F, Gutman F, Giannesini C, Penicaud A, Galanaud D, Kerrou K et al (2008) MR and FDG PET/TC findings in a case of probable Heidenhain variant Creutzfeldt–Jacob disease. J Neuroradiol 35:240–243
Krasnianski A, Kallenberg K, Collie DA, Meissner B, Schulz-Scaeffer WJ, Heinemann U et al (2008) MRI in the classical MM1 and the atypical MV2 subtypes of sporadic CJD: an inter-observer agreement study. Eur J Neurol 15:762–771
Poon MA, Stuckey S, Storey E (2001) MRI evidence of cerebellar and hippocampal involvement in Creutzfeldt–Jakob disease. Neuroradiology 43(9):746–749
Chang CC, Eggers SD, Johnson JK, Haman A, Miller BL, Geschwind MD (2007) Anti-GAD antibody cerebellar ataxia mimicking Creutzfeldt–Jakob disease. Clin Neurol Neurosurg 109(1):54–57
Sureka J, Jakkani RK (1017) Clinico-radiological spectrum of bilateral temporal lobe hyperintensity: a retrospective review. Br J Radiol 2012(85):e782–e792
Küker W (2007) Cerebral vasculitis: imaging signs revisited. Neuroradiology 49(6):471–479
Gomes LJ (2010) The role of imaging in the diagnosis of central nervous system vasculitis. Curr Allergy Asthma Rep 10(3):163–170
Thurnher MM, Donovan Post MJ (2008) Neuroimaging in the brain in HIV-1-infected patients. Neuroimaging Clin N Am 18(1):93–117
Ito H, Mori K, Kagami S (2011) Neuroimaging of stroke-like episodes in MELAS. Brain Dev 33(4):283–288
Hegde AN, Mohan S, Lath N, Lim CC (2011) Differential diagnosis for bilateral abnormalities of the basal ganglia and thalamus. Radiographics 31(1):5–30
Cianfoni A, Caulo M, Cerase A, Della Marca G, Falcone C, Di Lella GM et al (2013) Seizure-induced brain lesions: a wide spectrum of variably reversible MRI abnormalities. Eur J Radiol 82(11):1964–1972
Howard SA, Barletta JA, Klufas RA, Saad A, De Girolami U (2009) Best cases from the AFIP: osmotic demyelination syndrome. Radiographics 29(3):933–938
Cerase A, Rubenni E, Rufa A, Vallone I, Galluzzi P, Coratti G et al (2011) CT and MRI of Wernicke’s encephalopathy. Radiol Med 116(2):319–333
Rossi A (2008) Imaging of acute disseminated encephalomyelitis. Neuroimaging Clin N Am 18(1):149–161
Cardaioli E, Da Pozzo P, Cerase A, Sicurelli F, Malandrini A, De Stefano N et al (2006) Rapidly progressive neurodegeneration in a case with the 7472insC mutation and the A7472C polymorphism in the mtDNA tRNA ser(UCN) gene. Neuromuscul Disord 16(1):26–31
Reisin RC, Romero C, Marchesoni C, Napoli G, Kisinovsky I, Caceres G et al (2011) Brain MRI findings in patients with Fabry disease. J Neurol Sci 305(1–2):41–44
Politei JM, Capizzano AA (2006) Magnetic resonance image findings in 5 young patients with Fabry disease. Neurologist 12(2):103–105
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study is not funded.
Conflict of interest
We have no conflict of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gaudino, S., Gangemi, E., Colantonio, R. et al. Neuroradiology of human prion diseases, diagnosis and differential diagnosis. Radiol med 122, 369–385 (2017). https://doi.org/10.1007/s11547-017-0725-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-017-0725-y