Abstract
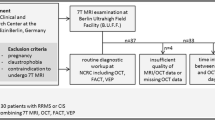
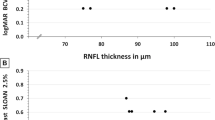
Monitoring disease burden is an unmeet need in multiple sclerosis (MS). Identifying patients at high risk of disability progression will be useful for improving clinical-therapeutic decisions in clinical routine. To evaluate the role of visual field testing in non-optic neuritis eyes (non-ON eyes) as a biomarker of disability progression in MS. In 109 patients of the MS-VisualPath cohort, we evaluated the association between visual field abnormalities and global and cognitive disability markers and brain and retinal imaging markers of neuroaxonal injury using linear regression models adjusted for sex, age, disease duration and use of disease-modifying therapies. We evaluated the risk of disability progression associated to have baseline impaired visual field after 3 years of follow-up. Sixty-two percent of patients showed visual field defects in non-ON eyes. Visual field mean deviation was statistically associated with global disability; brain (normalized brain parenchymal, gray matter volume and lesion load) and retinal (peripapillary retinal nerve fiber layer thickness and macular ganglion cell complex thickness) markers of neuroaxonal damage. Patients with impaired visual field had statistically significative greater disability, lower normalized brain parenchymal volume and higher lesion volume than patients with normal visual field testing. MS patients with baseline impaired VF tripled the risk of disability progression during follow-up [OR = 3.35; 95 % CI (1.10–10.19); p = 0.033]. The association of visual field impairment with greater disability and neuroaxonal injury and higher risk of disability progression suggest that VF could be used to monitor MS disease burden.
Similar content being viewed by others
References
Martínez-Lapiscina E, Sanchez-Dalmau B, Fraga-Pumar E et al (2014) The visual pathway as a model to understand brain damage in multiple sclerosis. Multiple Scler 20:1678–1685
Castro SMC, Damasceno A, Damasceno BP et al (2013) Visual pathway abnormalities were found in most multiple sclerosis patients despite history of previous optic neuritis. Arq Neuropsiquiatr 71:437–441
Gabilondo I, Martínez-Lapiscina EH, Martínez-Heras E et al (2014) Trans-synaptic axonal degeneration in the visual pathway in multiple sclerosis. Ann Neurol 75:98–107
Heesen C, Böhm J, Reich C et al (2008) Patient perception of bodily functions in multiple sclerosis: gait and visual function are the most valuable. Multiple Scler 14:988–991
Mowry EM, Loguidice MJ, Daniels AB et al (2009) Vision related quality of life in multiple sclerosis: correlation with new measures of low and high contrast letter acuity. J Neurol Neurosurg Psychiatry 80:767–772
Balcer LJ, Baier ML, Cohen JA et al (2003) Contrast letter acuity as a visual component for the multiple sclerosis functional composite. Neurology 61:1367–1373
Martínez-Lapiscina EH, Ortiz-Pérez S, Fraga-Pumar E et al (2014) Colour vision impairment is associated with disease severity in multiple sclerosis. Multiple Scler 20:1207–1216
Cheng H, Laron M, Schiffman JS et al (2007) The relationship between visual field and retinal nerve fiber layer measurements in patients with multiple sclerosis. Invest Ophthalmol Vis Sci 48:5798–5805
Keltner JL, Johnson CA, Cello KE, Dontchev M (2014) Visual field profile of optic neuritis (a final follow-up report from the optic neuritis treatment trial from baseline through 15 years). Arch Ophthalmol 128:330–337
Nevalainen J, Krapp E, Paetzold J et al (2008) Visual field defects in acute optic neuritis–distribution of different types of defect pattern, assessed with threshold-related supraliminal perimetry, ensuring high spatial resolution. Graefes Arch Clin Exp Ophthalmol 246:599–607
Chorazy M, Drozdowski W, Sherkawey N, Mariak Z (2007) Asymptomatic visual field disturbances in multiple sclerosis patients without a history of optic neuritis. Neurol Neurochir Pol 41:223–228
Martínez-Lapiscina EH, Fraga-Pumar E, Gabilondo I et al (2014) The multiple sclerosis visual pathway cohort: understanding neurodegeneration in MS. BMC Res Notes. doi:10.1186/1756-0500-7-910
Polman CH, Reingold SC, Edan G et al (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Martínez-Lapiscina EH, Fraga-Pumar E, Pastor X et al (2014) Is the incidence of optic neuritis rising? Evidence from an epidemiological study in Barcelona (Spain), 2008–2012. J Neurol 261:759–767
Petzold A, Wattjes MP, Costello F et al (2014) The investigation of acute optic neuritis: a review and proposed protocol. Nat Rev Neurol 10:447–458
Cohen JA, Barkhof F, Comi G et al (2010) Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med 362:402–415
Rudick RA, Polman CH, Cohen JA et al (2009) Assessing disability progression with the multiple sclerosis functional composite. Multiple Scler 15:984–997
Birt CM, Shin DH, Samudrala V et al (1997) Analysis of reliability indices from humphrey visual field tests in an urban glaucoma population. Ophthalmology 104:1126–1130
Keltner JL, Johnson CA, Cello KE et al (2003) Classification of visual field abnormalities in the ocular hypertension treatment study. Arch Ophthalmol 121:643–650
Yushkevich PA, Piven J, Hazlett HC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128
Sdika M, Pelletier D (2009) Nonrigid registration of multiple sclerosis brain images using lesion inpainting for morphometry or lesion mapping. Hum Brain Mapp 30:1060–1067
De Stefano N, Airas L, Grigoriadis N et al (2014) Clinical relevance of brain volume measures in multiple sclerosis. CNS Drugs 28:147–156
Saidha S, Al-Louzi O, Ratchford JN et al (2015) Optical coherence tomography reflects brain atrophy in multiple sclerosis: a four-year study. Ann Neurol 78:801–813
Sriram P, Wang C, Yiannikas C et al (2014) Relationship between optical coherence tomography and electrophysiology of the visual pathway in non-optic neuritis eyes of multiple sclerosis patients. PLoS One 9:e102546. doi:10.1371/journal.pone.0102546
Villoslada P, Cuneo A, Gelfand J et al (2012) Color vision is strongly associated with retinal thinning in multiple sclerosis. Multiple Scler 18:991–999
Trip SA, Schlottmann PG, Jones SJ et al (2005) Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol 58:383–391
Kitsos G, Detorakis ET, Papakonstantinou S et al (2011) Perimetric and peri-papillary nerve fibre layer thickness findings in multiple sclerosis. Eur J Neurol 18:719–725
Walter SD, Ishikawa H, Galetta KM et al (2012) Ganglion cell loss in relation to visual disability in multiple sclerosis. Ophthalmology 119:1250–1257
Lampert EJ, Andorra M, Torres-Torres R et al (2015) Color vision impairment in multiple sclerosis points to retinal ganglion cell damage. J Neurol 262:2491–2497
Friese MA, Schattling B, Fugger L (2014) Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat Rev Neurol 10:225–238
Laron M, Cheng H, Zhang B et al (2010) Comparison of multifocal visual evoked potential, standard automated perimetry and optical coherence tomography in assessing visual pathway in multiple sclerosis patients. Multiple Scler 16:412–426
Schinzel J, Zimmermann H, Paul F et al (2014) Relations of low contrast visual acuity, quality of life and multiple sclerosis functional composite: a cross-sectional analysis. BMC Neurol 14:31
Baier ML, Cutter GR, Rudick RA et al (2005) Low-contrast letter acuity testing captures visual dysfunction in patients with multiple sclerosis. Neurology 64:992–995
Castro DPE, Kawase J, Melo LAS (2008) Learning effect of standard automated perimetry in healthy individuals. Arq Bras Oftalmol 71:523–528
Acknowledgments
We are extremely grateful to the MS-VisualPath participants and fieldworkers without whose contribution, this study would not be possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data
Elena H. Martínez-Lapiscina had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This study was supported by Instituto de Salud Carlos III, Spain: PS09/00259 and RD07/0060/01 to PV and RD12/0032/0002 to AS. EHML was supported by a fellowship from the Instituto de Salud Carlos III, Spain (Rio Hortega Program: CM13/00150). The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
AS has received compensation for consulting services and speaking from Bayer-Schering, Merck-Serono, Biogen-Idec, Sanofi-Aventis, Teva Pharmaceutical Industries Ltd and Novartis. PV has received consultancy fees from Heidelberg Engineering regarding the clinical applications of optical coherence tomography. Elena H Martinez-Lapiscina has received for speaking honoraria from Biogen Idec and Genzyme and travel reimbursement from TEVA for The European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) and Sociedad Española de Neurología (SEN) and from Bayer Healthcare for American Academy of Neurology (AAN) over the last 3 years. All other authors have no conflicts of interest to declare.
Ethical standard
This means that the study has compliance with ethical standars which is a key requirement to obtain the approval by the mentioned committee.
Informed consent
It is stated in methods that Hospital Clinic of Barcelona Institutional Review Board approvals were obtained and all participants provided written informed consent.
Rights and permissions
About this article
Cite this article
Ortiz-Perez, S., Andorra, M., Sanchez-Dalmau, B. et al. Visual field impairment captures disease burden in multiple sclerosis. J Neurol 263, 695–702 (2016). https://doi.org/10.1007/s00415-016-8034-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8034-2