Abstract
Purpose
American Indian/Alaska Native (AI/AN) populations have some of the lowest cancer screening rates compared to other racial/ethnic populations. Using community-based participatory research methods, we sought to characterize knowledge, attitudes, beliefs, and approaches to enhance breast, colorectal, and cervical cancer screening.
Methods
We conducted 12 focus groups between October 2018 and September 2019 with 96 eligible AI adults and healthcare providers, recruited using non-probability purposive sampling methods from the Zuni Pueblo in rural New Mexico. We used the Multi-level Health Outcomes Framework (MHOF) to conduct a qualitative content analysis identifying mutable systems- and individual- level constructs important for behavior change that we crosslinked with the Community Preventive Services Task Force (CPSTF) recommended evidence-based interventions (EBIs) or approaches.
Results
Salient systems-level factors that limited uptake of cancer screenings included inflexible clinic hours, transportation barriers, no on-demand service and reminder systems, and brief doctor–patient encounters. Individual-level barriers included variable cancer-specific knowledge that translated into fatalistic beliefs, fear, and denial. Interventions to enhance community demand and access for screening should include one-on-one and group education, small media, mailed screening tests, and home visitations by public health nurses. Interventions to enhance provider delivery of screening services should include translation and case management services.
Conclusions
The MHOF constructs crosslinked with CPSTF recommended EBIs or approaches provided a unique perspective to frame barriers and promoters of screening utilization and insights for intervention development. Findings inform the development of culturally tailored, theoretically informed, multi-component interventions concordant with CPSTF recommended EBIs or approaches aimed at improving cancer screening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, the United States has witnessed a steady decline in overall cancer incidence (especially for men) and mortality, and an improvement in 5-year relative survival [1]. These gains, however, have not accrued evenly across populations. American Indian/Alaska Native (AI/AN) populations compared with non-Hispanic Whites (NHWs) have experienced persistent disparities in cancer incidence, mortality, and survival [2, 3]. Cancer disparities among the AI population in New Mexico (NM) are equally concerning (Note: when referring to NM-specific data, we use the abbreviation “AI” referring to American Indians only and not “AN” which includes Alaska Natives). Between 2012 and 2016, compared with the state’s NHW population, AI females had higher cervical and colorectal cancer incidence and higher cervical cancer mortality [4], while AI males had higher colorectal cancer incidence and mortality [4]. The state’s AI population was also more likely to receive diagnosis at a later stage (i.e., regional or distant) for all three cancers [5].
AI/AN populations have some of the lowest screening rates for the three screen-detectable (i.e., breast, colon-rectum, cervical) cancers compared to other racial/ethnic populations. In NM, the AI population in the Indian Health Service (IHS) Albuquerque Area compared with the state’s NHW population has substantially lower screening for breast (38.7% vs. 70.0%) [6, 7], colorectal (31.2% vs. 69.2%) [6, 8], and cervical (43.3% vs. 77.8%) [6, 9] cancers. AI/AN populations experience substantial individual-, and provider-/system-level barriers accessing screening services. These barriers include historical mistrust about healthcare services and institutions [10,11,12]; discordant patient–provider gender roles [11,12,13]; hesitancy to discuss cancer [14, 15]; privacy and confidentiality concerns [13, 16]; perceptions of not receiving quality and competent care [17]; fatalistic views about cancer [15, 18]; and no cultural or social norms for screening [19]. Further, Tribes and the IHS possess limited healthcare resources to address cancer disparities as healthcare is severely underfunded, services are often fragmented, and acute care needs take precedence over preventive care [20, 21].
Persistent cancer health disparities coupled with barriers to access and delivery of cancer screening for AI/AN populations argue for tailored, theoretically informed, multicomponent evidence-based interventions (EBIs) or approaches to enhance screening. The Community Preventive Services Task Force (CPSTF) has recommended EBIs or approaches to promote breast [22, 23], colorectal [22, 24], and cervical [22, 25] cancer screening. EBIs or approaches with “strong evidence” for effectiveness to enhance screening for these three cancers include multicomponent interventions, interventions engaging community health workers or navigators, client-oriented interventions (e.g., incentives, one-on-one education, and small media), and provider-oriented interventions (e.g., assessment and feedback, and reminder and recall systems).
With one exception [15], none of the research reviewed above on cancer and cancer screening perspectives was conducted among NM’s AI population. The diversity of AI/AN populations across the US, including 573 federally recognized Tribes [26] speaking about 150 Tribal languages [27], provides a compelling rationale to elicit representatively diverse perspectives from a broad range of AI/AN populations. The purpose of this qualitative inquiry that used a community-based participatory research (CBPR) approach was three-fold. First, using qualitative methods, elicit perspectives on knowledge, attitudes, and beliefs regarding the prevention and control of the three screen-detectable cancers among the AI population residing in the Zuni Pueblo in rural NM and among healthcare providers practicing at the Zuni IHS Comprehensive Health Center (hereafter, “Health Center”). Second, theoretically ground these perspectives with constructs of the Multi-level Health Outcomes Framework (MHOF) [28,29,30]. Identification of mutable individual- and system-level factors, such as knowledge, attitudes, beliefs, structural barriers, provider reminders and recall systems, and navigation services are particularly important as they represent potential targets for intervention. Third, map the perspectives and MHOF constructs on to the CPSTF recommended EBIs or approaches for potential multicomponent interventions.
Material and methods
Study setting and sample
We conducted the research at the UNM Health Sciences Center (HSC) satellite office and the Health Center, located on the Zuni Pueblo. The UNM HSC’s Human Research Review Committee and the Southwest Tribal Institutional Review Board approved all aspects of the research protocol. Eligibility criteria included adults (21–75 years) who self-identified as tribal members and resided in the Pueblo. Consistent with principles of qualitative research methodology, we used non-probability (non-random) purposive sampling techniques [31] to identify and invite eligible community members and healthcare providers for the focus groups. We identified community members based on recommendations from the Tribal Advisory Panel (TAP) and word of mouth, and recruited them based on selected characteristics (i.e., age, gender). Further, TF used the same sampling technique to invite healthcare providers practicing at the Health Center to the focus group. These healthcare providers included those who expressed an interest in the study topic, were primary care providers, and did not have clinical or administrative responsibilities at the time of the focus group.
The Health Center is the only healthcare facility located on the Zuni Pueblo. It provides standard cancer screenings on a routine basis to all age-eligible patients being seen for primary care. These include digital mammogram for breast cancer (ultrasound for diagnostic breast exams), Pap smear for cervical cancer, and immunochemical fecal occult blood testing or colonoscopy referral (based on patient preference) for colorectal cancers. The Health Center does not offer mammography mobile vans, self-sampling for cervical cancer screening, and colonoscopies. Patients are referred over two hours away to Albuquerque for colonoscopies, with wait times for scheduling them often six to nine months. It is open 24/7, has evening primary care clinic hours, provides option to the patients to choose gender concordant providers, and has an appointment reminder system.
Theoretical framework
The MHOF [28,29,30] informed the discussion guide and analysis approach. It has been used to study antecedents of health behavior in diverse cancer control studies [29, 30, 32,33,34,35,36,37,38]. We elicited participants’ perspectives on several modifiable individual- and system-level MHOF constructs with a view of integrating these constructs in cognitive-behavioral interventions. The MHOF originates outside the cultural context of Zuni and serves as a guiding framework that will be adapted and revised based on emerging data.
Community-based participatory research
We employed engagement processes founded on CBPR principles, which envision researchers and community members establishing a non-hierarchical partnership for all phases of the research [39,40,41]. CBPR is a necessary methodology for research with AI/AN populations [42,43,44,45] as it addresses mistrust of research and researchers. Zuni project staff and students provided critical input on all aspects of the research. Tribal leaders, recruited to the Tribal Advisory Panel (TAP), shared their expertise on development of the focus group guide, participant recruitment strategies, and interpretation of findings. We tailored protocols for cultural acceptability and respectfulness, and built sustainable processes for long term impact of the project.
Focus group procedures
We convened three clusters of eligible AI community members, stratified by age and gender. These clusters included: females ages 21–49 years for discussions on cervical cancer and HPV, females ages 50–75 years for discussions on breast, colorectal, and cervical cancers, and HPV, and males ages 50–75 years for discussions on colorectal and prostate cancers. In this report, for men 50–75 years, we only analyze and present focus group discussions on colorectal cancer. Zuni research assistants (SL, TB, KH, KB) or the first author moderated the discussions with community members. ALS moderated the discussions with healthcare providers. The discussions were primarily in English, although there were instances when community members spontaneously conversed in the Zuni language, “Ashiwi awan benawe.” We ended data collection after reaching thematic saturation [46, 47]. At the end of each discussion, the first author addressed misconceptions raised during the discussions. Participants completed a socio-demographic survey prior to the discussion. They received merchandize cards based on the time commitment of their respective groups. Men and women ages 50–75 years received $75 merchandize cards for groups that averaged about 90 min; women ages 21–49 years and the providers received $50 merchandize cards for groups that averaged about 60 min.
We conducted 12 focus groups [48] between October 2018 and September 2019, with each group comprising 4–13 participants. The moderator followed a discussion guide (available upon request) specific to the community member’s age/gender strata and the healthcare providers. The guides explored individual- and systems-level facilitators and barriers to cancer screening, and strategies that can enhance screening behavior. For the community member focus groups, the key areas of inquiry included knowledge about the specific cancer (i.e., risk factors, prevention); perceptions of susceptibility to and severity of cancer; personal and family history of cancer; knowledge about and use of cancer-specific screening test; social support and social norms for cancer screening; communications with healthcare providers regarding cancer and cancer screening; cultural and traditional beliefs regarding cancer; and strategies to enhance screening. For the healthcare provider focus group, the key areas of inquiry included their perceptions of the community’s beliefs and attitudes regarding preventive behaviors and cancer prevention, help-seeking behavior, and knowledge about cancer; providers’ approaches and experiences with counseling patients about cancer screening; challenges to providing cancer screening; and potential strategies to improve cancer screening in the community. Stem questions emphasized a strengths-based approach [49, 50] for identifying solutions to barriers and potential health-promoting intervention strategies. The purposive sampling technique employed in addition to iterative data collection and analysis, leading to data saturation, generate confidence that the findings of the research will serve as the basis for testable interventions. Moreover, through systematic and rigorous application of qualitative methods, findings of this research will be conceptually and culturally relevant.
Data analysis
Pairs of research assistants, conversant in both English and “Ashiwi awan benawe,” transcribed verbatim the audio recording and verified the transcription. Transcripts and the note-taker’s observations served as the primary data sources. We employed a sequential approach to our analysis, importing transcripts, coding, and querying using NVivo 10, a qualitative data analysis software program. First, we used a systematic iterative process to code transcripts for the MHOF constructs to ground the participants’ perspectives within the theoretical framework. In all, we coded the transcripts for 16 MHOF constructs, besides potential intervention strategies discussed by the participants. We then identified preliminary and emergent themes of importance for each MHOF construct. Several team members independently read each transcript to identify preliminary findings, which facilitated confirmation of emergent themes. The initial analysis resulted in a coding template consisting of 40–53 themes and subthemes depending on the age/gender or provider cluster. After coding all transcripts, we queried the database by coding categories for more refined interpretive analyses. Next, we cross-linked the emergent themes to the CPSTF EBIs or approaches to ground the analyses in actionable EBIs or approaches backed by “strong evidence” for effectiveness to enhance screening for the cancers under study. Lastly, we presented our preliminary findings to the TAP and Zuni Tribal Council members for their interpretation of the findings and data narratives. We analyzed the quantitative survey data to produce descriptive assessments of the participants’ demographics.
Results
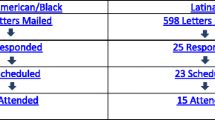
Table 1 presents socio-demographic characteristics on 85 community members and 11 healthcare providers who participated in the focus groups. The majority of community members were Zuni tribal members (with three participants having non-Zuni tribal affiliation), spoke “Ashiwi awan benawe” either often or always, were mostly single, high school graduates or college educated, in the workforce, and had health insurance. Although IHS does not provide health insurance, nearly one-quarter of the community members indicated IHS as their health insurance. This interpretation may be due to community members’ reliance on IHS for all their health care and costs. The majority of healthcare providers were young [30,31,32,33,34,35,36,37,38,39 years], female, NHW persons, specialized in family medicine, and had been in medical practice for less than 5 years.
We have organized the results in two sections. Section I links community member and provider perspectives with selected MHOF constructs, and Section II, building on the strengths-based approach, links community members’ suggested interventions to enhance screening with the CPSTF recommended EBIs or approaches.
-
I.
Community Member and Provider Perspectives Linked with Selected MHOF Constructs
We organized results by three MHOF constructs: knowledge, barriers and supports (e.g., community member, provider, system, society), and communications (including communication with providers and with others). We have included exemplary quotes below and Table 2 presents additional quotes supporting each construct.
-
1.
Knowledge
Across the groups, community members consistently reported variable knowledge and awareness regarding cancer etiology, specific cancer types, and associated screening tests. Community members cited a need for clear information about different cancers, screening tests, and prevention strategies (Table 2, quotes C1-C2). In response to questions about potential causes of cancer, community members expressed a range of views pertaining to causal possibilities, including environmental contributors (e.g., airborne contaminants and water), food sources attributable to dietary changes over time, and heredity (Table 2, quotes C3-C6).
When aware or informed, community members reported receptivity to preventive strategies such as HPV vaccinations and screening (Table 2, quote C7).
“Screening is really important. So that way at least there [will] hopefully [be] some […] intervention, prevention awareness that most people will start understanding.” (Men 50-75)
Providers generally concurred, noting that while community members maintained a basic knowledge of cancer, they attributed low screening rates to individual- and system-level barriers discussed below under barriers and supports. Providers indicated that community members wanted to know about cancer and screening, especially if they had to help or take care of a family member who had cancer or had a family history (Table 2, quotes P1-P2). As a provider noted:
“I think there are some patients who definitely want to know if they have cancer. I think people who have family history, whether its siblings, parents are kind of more interested because they worry that it could be affecting them.”
-
2.
Barriers and Supports
Community members cited systemic barriers giving rise to frustration (Table 2, quote C8), fear of cancer diagnosis (Table 2, quote C9), and embarrassment given test procedures (e.g., Pap test, stool test) (Table 2, quote C10) and concerns pertaining to confidentiality given the likelihood of potential interactions with medical staff who may be neighbors or family members.
“For me it…was really the embarrassment because there’s a lot of [local] nurses now and I don’t want another [local resident] looking at me down there.” (Women 21–49)
“Well…it’s confidentiality. That’s what I was worried about. Our people are nosey. When you walk into the hospital you’ll get stared at hard.” (Men 50–75)
Community members also identified the benefits of supportive elements (i.e., family members) to promote better health and overcome screening hesitancy and embarrassment (Table 2, quotes C11-C12).
Providers echoed interrelated concepts of fear/denial, fatalism, and procrastination as barriers to cancer screening (Table 2, quotes P3-P5).
“It’s on people’s radars…it’s on the back of their minds, but [there is] a very strong denial…”
Providers described social determinants of health as important barriers. Further, providers reflected on competing priorities (i.e., financial insecurity, child care, stress) among their patients given social conditions of poverty and other demands (Table 2, quote P6).
Providers mentioned additional systems-level barriers that precluded access to timely screenings. These included transportation issues, long wait times at clinics, inflexible clinic hours, inability to provide screening on-demand, lack of child care, lack of reminder systems (for patients and providers), limitations of the Electronic Health Record (EHR) system, and no system or procedures in place to collect completed stool kits (Table 2, quotes P7-P11).
-
3.
Communication
We explored levels of communication to discern the degree to which one’s social network influenced perspectives on screening behaviors as well as self-reported interactions with healthcare providers. With regard to social networks, community members indicated the importance and need for discussing health behaviors and cancer screening with family members (Table 2, quote C13):
“… whatever you’re told [from the doctor about being diagnosed with cancer], you know, I would go home and discuss it with my family to let them know what’s going [on]…” (Women 50–75)
“…in order to break the cycle you have to sit and do not be afraid, not be ashamed, not be embarrassed, but to seriously talk about it.” (Women 21–49)
Community members expressed that the use of humor, confidence and trust in the provider, and gender concordance with their provider eased communications of serious issues (Table 2, quotes C14-C17). Community members, however, attributed a lack of conversation about topics such as cancer, cancer screening, and death to generalized cultural traditions, gender norms, and privacy concerns (Table 2, quotes C18-C20). Additionally, systems-level factors precluded expanded discussions on healthcare needs. These factors included brief clinic visits and use of medical jargon and, which may be a function of insufficient clinic manpower or lack of prioritization of cancer screening at the clinic (Table 2, quotes C21-C22).
Providers emphasized prioritizing communication with patients about cancer screening as they mostly attributed low screening rates to patient choices and lack of follow-through. They noted in their patients an awareness about and desire to act on the need for screening but not going through it (Table 2, quotes P12-P13). A provider also noted the cultural taboo limiting discussion about cancer within family contexts (Table 2, quote P14).
Providers indicated that they utilize culturally tailored counseling strategies in recognition of the need to address cancer screening in an indirect manner (i.e., communicating in third person) (Table 2, quote P15), a strategy also employed by their patients (Table 2, quote P16). Providers also use humor to communicate the importance of the test (Table 2, quote P17).
-
II.
Building on the Strengths-Based Approach, Linking Community Members’ Suggested Interventions to Enhance Screening with The CPSTF Recommended EBIs or Approaches
Building on the strengths-based approach, we cross-referenced major thematic findings derived from community member and provider focus groups with the CPSTF recommended EBIs or approaches to guide identification of interventions or approaches aligned with community perspectives (Table 3). We limited our analyses to CPSFT recommended EBIs or approaches that have “strong evidence” in support of their effectiveness (previously described). Further, we aligned the interventions or approaches with the MHOF constructs presented in Table 2.
-
1.
Potential Client-Oriented Interventions
Community members endorsed a series of interventions or approaches to increase demand for screening services. They advocated one-on-one and group education interactions led by community health workers (i.e., field nurse, public health nurse, or other healthcare professional) to increase awareness and address knowledge gaps. They noted that offering both types of educational sessions ensures alignment with community member preferences. Further, they suggested systems-level approaches that addressed transportation barriers, such as having field health nurses provide education around screening to community members in their homes, offer to pick up stool test kits (Table 3; quotes 1–6).
“One-on-one [sessions would be best to encourage people to get screened], so that way they’ll be just there with the person and however they’re feeling they’ll do everything that is asked of them…without having to be afraid of the people that are sitting in there. Maybe if it’s crowded like this [focus group] they’ll be embarrassed and they won’t ask a lot of questions...” (Women 50-75)
In response to concerns expressed about healthcare services at facilities where they sought care, community members supported systems-level solutions such as a scheduling system or client reminders about appointments. In addition to serving a pragmatic purpose, reminders were also viewed as a sign that the healthcare facilities were invested in community members’ wellbeing. (Table 3; quote 7).
“…schedule appointments ahead of time and maybe people will make arrangements to keep their appointments…” (Women 50–75)
“I was supposed to go [to the urologist last year] but…I don’t know why they…rescheduled my appointment so I had to reschedule my appointment then and I haven’t gone [back].” (Men 50–75)
Use of small media, including pamphlets and flyers, were suggested by community members as an educational strategy. (Table 3; quotes 8–9) Lastly, to increase access to screening by reducing structural barriers, community members emphasized systems-level strategies such as flexible and responsive appointment scheduling and assistance, and as needed, overcoming transportation barriers. (Table 3; quotes 10–12).
-
2.
Potential Provider-Oriented Interventions
Community members noted challenges to provider communication or, in some situations, perceived lack of empathy (e.g., the provider not spending sufficient time with the patient or brushing aside the patient’s concerns). They also noted translation and case management services could improve doctor–patient communication. (Table 3; quotes 13–15).
“Sometimes…you don’t understand what the doctor is saying to you. It’s hard to understand, and you repeat it in your own way and then I don’t know…” (Men 50–75)
Discussion
The goal for this CBPR-informed research conducted with AI community members and providers in rural NM was to identify salient and mutable MHOF constructs, crosslinking them with CPSTF recommended EBIs or approaches, to subsequently design and implement a multicomponent intervention to enhance cancer screening rates. We identified important systems-level barriers that limited community access to screening services at healthcare facilities the community members seek care (which may not be the Health Center located on the Zuni Pueblo). These included inflexible clinic hours, inadequate provider communications, lack of transportation, privacy/confidentiality concerns, lack of gender concordant provider, need for translation and case management services, and the need for patient and provider reminder systems.
Strategies to enhance community demand for and access to screening should include one-on-one and group education, use of small media, and interactions with and home visitations by community health workers. These educational strategies should focus on the specific cancer type and their screening modalities. Strategies to enhance provider delivery of screening services should include the provision of translation and case management services. Although cultural norms generally preclude discussion about cancer or medical history among family members and friends, there appears to be some effort in the Zuni community to transcend this taboo. Community members and providers cited several instances of open communications regarding cancer and screening tests among family members and with providers.
The findings corroborate those documented from qualitative studies among AI/AN populations across the US on cancer screening [10,11,12,13,14,15,16,17,18]. Similar to the findings reported here, those studies also documented hesitancy to discuss cancer and cancer screening, negative experiences with the healthcare system, transportation barriers, fear of screening results, lack of quality and competent care, and concerns about privacy and embarrassment. This research extends these findings by documenting important individual- and systems-level barriers and supports for screening. Individual-level factors to support screening included the willingness to act on information, a growing willingness to discuss cancer and cancer screening with family members, trust in healthcare providers, and receiving gender concordant care. Systems-level barriers encountered where community members sought healthcare services included frustration with healthcare providers, inflexible clinic hours and the need for on-demand service, need for translation and case management services, limitations of the EHR system, and no patient and provider reminder systems.
Community members identified several CPSTF recommended EBIs or approaches to enhance screening that would work well in the context of their community, cultural preferences, and healthcare environment. Potential client-oriented EBIs or approaches to improve community demand included enhancing knowledge through culturally appropriate one-on-one and group education; however, the rationale for each strategy was quite different. One-on-one education and interactions with public health nurses could ensure privacy, while home visitations and mailed screening tests (for colorectal and cervical cancers) would address the lack of transportation as a structural barrier. Group education was recommended to address knowledge as some community members felt empowered to leave behind their fears and taboos and openly discuss cancer and its implications in such a setting. Further, group education could lead to one-on-one discussions with family members. Small media would complement these educational strategies. Additional intervention strategies could include translation and case management services to address poor or brief doctor–patient communications and interactions. Providers highlighted that cultural taboos limited discussions around cancer within the family context. They circumvented this by utilizing culturally tailored communication strategies such as using gentler phrases such as colorectal “health” instead of colorectal “cancer” or talking in the third person (a strategy also employed by community members). Providers expressed the need to use humor when discussing important health-related topics. To the extent that the community members identified CPSTF recommended EBIs or approaches [22,23,24,25] that are also endorsed by other populations is indicative that similar interventions or approaches may be appropriate across broad populations. At the same time, a long history of research has underscored the importance of “cultural tailoring” of interventions to reflect the cultural context, norms, and mores of different populations [51,52,53]. This tailoring could be through inclusion of culturally appropriate language and communication strategies, art, testimonials, and role models.
The diversity of AI/AN populations argue for the importance and need to document these perspectives from AI/AN populations across the US to better inform indigenous narratives around health. The current study is unique for its contributions as one of the first studies in AI/AN populations to document and contrast cancer control and prevention perspectives elicited from community members and healthcare providers practicing in the same community, and to link these perspectives to modifiable constructs of the MHOF and CPSTF recommended EBIs or approaches for intervention development. The focus group format allowed us to discover the tension between the desire to take charge of one’s health and systems-level, cultural or affective reasons for not doing so.
Our study has strengths and limitations. A compelling strength of this study is the use of a theoretical framework (MHOF) to organize the qualitative data and link it with CPSTF recommended EBIs or approaches, thus making the data actionable in terms of potential multicomponent EBIs to enhance cancer screenings. Further, use of the MHOF has helped contextualize the findings within a larger body of literature. One of the MHOF’s construct is “cultural beliefs.” Given the population of interest for this research, the focus group guide included questions and probes to pursue this line of inquiry. However, cultural imperatives preclude talking about certain topics such as cancer, as documented in this study and elsewhere [15]. We recently documented no significant associations between health literacy/numeracy and cancer screening in the Zuni Pueblo, a finding not aligned with many studies [54]. We have postulated that “standard” questions used to assess health literacy may need to be tailored to the contextual and cultural realities of the populations under study. Another strength is implementation of the CBPR methodology that facilitated bi-directional partnerships with community members on all phases of the research. This engagement drives development of indigenous data narratives, commits to sustainability, and makes the research socially actionable to address the cancer control needs of the Zuni community. The findings from this qualitative study are based on one Tribal population and group of healthcare providers in one rural NM community. As such, they are not representative or fully generalizable to heterogeneous AI/AN populations across the US. The limited number of focus groups per age/gender clusters could further reduce generalizability of our findings. Despite the limited number of groups conducted, there was convergence on the main themes reported across the various clustered groups and we achieved thematic saturation on areas of inquiry. Given the breadth and depth of focus group discussions, what we may have lost in terms of generalizability based on the relatively small number of focus groups, we gained through contextually rich discussions.
In conclusion, the MHOF constructs linked with CPSTF recommended EBIs or approaches provided a unique perspective to frame barriers and promoters of screening uptake and insights to develop multicomponent EBIs. The insights gained from this qualitative research are being validated through a community-wide quantitative survey. These qualitative and quantitative data will be used for culturally tailored, theoretically informed, multicomponent interventions concordant with CPSTF recommended EBIs or approaches aimed at improving screenings for colorectal, breast, and cervical cancers among age-eligible men and women in the Zuni Pueblo in rural NM.
Data availability
The authors are committed to the open and timely dissemination of unique research outcomes in compliance with Tribal and federal (NIH) policies. The authors will share data being cognizant of the data sharing needs and goals of the participating Tribe, and are guided by the Tribal data sharing agreements.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Melkonian SC, Jim MA, Haverkamp D, Wiggins CL, McCollum J, White MC et al (2019) Disparities in Cancer Incidence and Trends among American Indians and Alaska Natives in the United States, 2010–2015. Cancer Epidemiol Biomarkers Prev 28(10):1604–1611
White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS (2014) Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health 104(Suppl 3):S377–S387
New Mexico Tumor Registry. Cancer in New Mexico. Albuquerque, NM: New Mexico Tumor Registry. Available at: http://nmtrweb.unm.edu/statistics/index.html. Accessed March 11, 2022.
New Mexico Tumor Registry. Opportunities for Cancer Control: an overview of screen-detectable and tobacco-related cancer in New Mexico. Albuquerque, New Mexico: New Mexico Tumor Registry, 2013. Available at: http://nmtrweb.unm.edu/_pdf/OpportunitiesForCancerControl.pdf. Accessed March 11, 2022.
U.S. Department of Health and Human Services, Indian Health Service. FY 2019 GPRA/GPRAMA IDCS National Results: Indian Health Service (IHS) GPRA Performance Results. Washington, DC: Indian Health Service. Available at: https://www.ihs.gov/sites/quality/themes/responsive2017/display_objects/documents/FY_2019_GPRA_GPRAMA_NationalandAreaResults.pdf. Accessed March 11, 2022.
New Mexico Department of Health. Health Indicator Report of Cancer Screening--Mammography. Santa Fe, NM: New Mexico Department of Health, Indicator-Based Information System for Public Health. Available at: https://ibis.health.state.nm.us/indicator/view/CancerScrMammo.RacEth.html. Accessed March 11, 2022.
New Mexico Department of Health. Health Indicator Report of Cancer Screening--Colorectal Cancer Screening. Santa Fe, NM: New Mexico Department of Health, Indicator-Based Information System for Public Health. Available at: https://ibis.health.state.nm.us/indicator/view/CancerScrColoRec.Age50-75.RacEth.html. Accessed March 11, 2022.
New Mexico Department of Health. Health Indicator Report of Cancer Screening--Pap Test. Santa Fe, NM: New Mexico Department of Health, Indicator-Based Information System for Public Health. Available at: https://ibis.health.state.nm.us/indicator/view/CancerScrPap.Age21-65.RacEth.html. Accessed March 11, 2022.
James AS, Filippi MK, Pacheco CM, Cully L, Perdue D, Choi WS et al (2013) Barriers to colorectal cancer screening among american Indian men aged 50 or older, kansas and missouri, 2006–2008. Prev Chronic Dis 10:E170
Daley CM, Filippi M, James AS, Weir M, Braiuca S, Kaur B et al (2012) American Indian community leader and provider views of needs and barriers to mammography. J Community Health 37(2):307–315
Daley CM, James AS, Filippi M, Weir M, Braiuca S, Kaur B et al (2012) American Indian community leader and provider views of needs and barriers to colorectal cancer screening. J Health Disparities Res Pract 5(2):2
Daley CM, Kraemer-Diaz A, James AS, Monteau D, Joseph S, Pacheco J et al (2012) Breast cancer screening beliefs and behaviors among American Indian women in Kansas and Missouri: a qualitative inquiry. J Cancer Edu 27(1 Suppl):S32-40
Filippi MK, Braiuca S, Cully L, James AS, Choi WS, Greiner KA et al (2013) American Indian perceptions of colorectal cancer screening: viewpoints from adults under age 50. J Cancer Edu 28(1):100–108
Safi S, Ghahate D, Bobelu J, Sussman AL, Rodman J, Wandinger-Ness A et al (2021) Assessing Knowledge and Perceptions About Cancer Among American Indians of the Zuni Pueblo. NM. J Cancer Edu. 4:160–166
Filippi MK, James AS, Brokenleg S, Talawyma M, Perdue DG, Choi WS et al (2013) Views, barriers, and suggestions for colorectal cancer screening among american Indian women older than 50 years in the midwest. J Prim Care Community Health 4(3):160–166
Filippi MK, Perdue DG, Hester C, Cully A, Cully L, Greiner KA et al (2016) Colorectal cancer screening practices among three American Indian communities in minnesota. J Cult Divers 23(1):21–27
Frerichs L, Rhode J, Bell R, Hunt C, Lowery J, Brooks M et al (2018) Perspectives of American Indians in Eastern North Carolina on Socio-cultural factors that influence colorectal cancer screening decisions. J Health Care Poor Underserved 29(2):723–742
James RD, Gold DE, John-BlackBird A, Brown TS (2015) Factors that influence mammography use among older American Indian and Alaska Native women. J Transcult Nurs 26(2):137–145
Warne D, Kaur J, Perdue D (2012) American Indian/Alaska Native cancer policy: systemic approaches to reducing cancer disparities. J Cancer Edu 27(Suppl 1):S18-23
U.S. Department of Health and Human Services, Indian Health Service. IHS Profile. Rockville, MD: Indian Health Service. Available at: https://www.ihs.gov/newsroom/factsheets/ihsprofile/. Accessed March 11, 2022.
The Guide to Community Preventive Services. CPSTF Findings for Cancer Prevention and Control. Available at: https://www.thecommunityguide.org/content/task-force-findings-cancer-prevention-and-control#cancerscreening. Page last updated: November 1, 2021. Accessed March 11, 2022.
The Guide to Community Preventive Services. Cancer Screening: Multicomponent Interventions--Breast Cancer. Available at: https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-breast-cancer. Page last updated: December 22, 2021. Accessed March 11, 2022.
The Guide to Community Preventive Services. Cancer Screening: Multicomponent Interventions--Colorectal Cancer. Available at: https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-colorectal-cancer. Page last updated: December 22, 2021. Accessed March 11, 2022.
The Guide to Community Preventive Services. Cancer Screening: Multicomponent Interventions--Cervical Cancer. Available at: https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-cervical-cancer. Page last updated: December 22, 2021. Accessed March 11, 2022.
U.S. Department of the Interior. Indian Affairs. Available at: https://www.bia.gov/frequently-asked-questions. Accessed March 11, 2022.
U.S. Census Bureau. Detailed Languages Spoken at Home and Ability to Speak English for the Population 5 Years and Over. Available at: https://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Accessed March 11, 2022.
Bastani R, Gallardo NV, Maxwell A (2001) Barriers to colorectal cancer screening among ethnically diverse high and average risk individuals. J Psychosoc Oncol 19:65–84
Bastani R, Glenn BA, Taylor VM, Chen MS Jr, Nguyen TT, Stewart SL et al (2010) Integrating theory into community interventions to reduce liver cancer disparities: the health behavior framework. Prev Med 50(1–2):63–67
Bastani R, Maxwell AE, Bradford C, Das IP, Yan KX (1999) Tailored risk notification for women with a family history of breast cancer. Prev Med 29(5):355–364
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K (2015) Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health 42(5):533–544
Mishra SI, Bastani R, Crespi CM, Chang LC, Luce PH, Baquet CR (2007) Results of a randomized trial to increase mammogram usage among Samoan women. Cancer epidemiol Biomarkers Prev 16(12):2594–2604
Mishra SI, Bastani R, Huang D, Luce PH, Baquet CR (2007) Mammography screening and Pacific Islanders: role of cultural and psychosocial factors. J Cancer Edu 22(1):32–36
Mishra SI, Luce PH, Baquet CR (2009) Increasing pap smear utilization among Samoan women: results from a community based participatory randomized trial. J Health Care Poor Underserved 20(2 Suppl):85–101
Glenn BA, Hamilton AS, Nonzee NJ, Maxwell AE, Crespi CM, Ryerson AB et al (2018) Obesity, physical activity, and dietary behaviors in an ethnically-diverse sample of cancer survivors with early onset disease. J Psychosoc Oncol 36(4):418–436
Lucas-Wright A, Duran P, Bazargan M, Vargas C, Maxwell AE (2019) Cancer-related knowledge, attitudes and behaviors within the latino faith community in South Los Angeles. Ethn Dis 29(2):239–246
Maxwell AE, Lucas-Wright A, Chang LC, Santifer RE, Crespi CM (2020) Factors associated with colorectal cancer screening in a peer-counseling intervention study in partnership with African American churches. Prev Med Rep 20:101280
Moucheraud C, Kawale P, Kafwafwa S, Bastani R, Hoffman RM (2020) “When You Have Gotten Help, That Means You Were Strong:” a qualitative study of experiences in a “Screen and Treat” program for cervical cancer prevention in Malawi. J cancer Edu. 37:405–413
Israel BA, Schulz AJ, Parker EA, Becker AB (1998) Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 19:173–202
Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R et al (2010) Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health 100(11):2094–2102
Wallerstein N, Duran B, Oetzel J, Minkler M (eds) (2017) Community-Based Participatory Research for Health: Advancing Social and Health Equity, 3rd edn. John Wiley & Sons, Hoboken, NJ
Burhansstipanov L, Christopher S, Schumacher SA (2005) Lessons learned from community-based participatory research in Indian country. Cancer control 12(Suppl 2):70–76
Kaur JS, Dignan M, Burhansstipanov L, Baukol P, Claus C (2006) The, “Spirit of Eagles” legacy. Cancer 107(8 Suppl):1987–1994
Dignan MB, Jones K, Burhansstipanov L, Michalek AM (2014) Evaluation lessons learned from implementing CBPR in Native American communities. J Cancer Edu 29(3):412–413
Noe TD, Manson SM, Croy C, McGough H, Henderson JA, Buchwald DS (2007) The influence of community-based participatory research principles on the likelihood of participation in health research in American Indian communities. Ethn Dis 17(1 Suppl 1):S6-14
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B et al (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 52(4):1893–1907
Guest G, Namey E, McKenna K (2016) How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods 29(1):3–22
Krueger RA, Casey MA (2009) Focus Groups: A Practical Guide for Applied Research (4th Edition). Sage Publciations, Inc, Thousand Oaks, CA
Mirkovic J, Kristjansdottir OB, Stenberg U, Krogseth T, Stange KC, Ruland CM (2016) Patient Insights Into the Design of Technology to Support a Strengths-Based Approach to Health Care. JMIR Res Protoc 5(3):e175
Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D et al (2007) Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med 33(3):221–235
Joo JY, Liu MF (2021) Culturally tailored interventions for ethnic minorities: A scoping review. Nurs Open 8(5):2078–2090
Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson V (2002) Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Edu Behav 30(2):133–146
Pasick RJ, D’onofrio CN, Otero-Sabogal R (2016) Similarities and differences across cultures: questions to inform A third generation for health promotion research. Health Edu Behav. 23(1):142–161
Cartwright K, Leekity S, Sheche J, Kanda D, Kosich M, Rodman J, et al. Health Literacy, Health Numeracy, and Cancer Screening Patterns in the Zuni Pueblo: Insights from and Limitations of "Standard" Questions. J Cancer Edu. 2022:1–11.
Acknowledgments
The authors gratefully acknowledge the Tribal stakeholders, including the Zuni Tribal Governor and his council members, as well as the Tribal Advisory Panel members who contributed to the study activities. The authors are also grateful to the Zuni people for welcoming us into their lives, and sincerely thank the men and women from the Zuni Pueblo and healthcare providers practicing at the Zuni IHS Comprehensive Health Center who participated in the focus groups. The authors also acknowledge the contributions of the University of New Mexico Health Sciences Center staff (Tanisha Boone [TB], Qiarra Lalio [QL], Kassie Hooee [KH], Kollin Bowannie [KB], Donica Ghahate, and Ellen Burgess) for assisting in conducting focus groups with community members and analyzing the qualitative data.
Funding
This research was supported by the UNM Comprehensive Cancer Center (UNMCCC) Support Grant NIH/NCI P30CA118100 (Tomkinson, PI), UNMCCC institutional pilot awards (PP-U1418-RS, PP-U1402-CaC, Mishra, PI), the UNMCCC Behavioral Measurement and Population Science Shared Resource, and the Institutional Development Award (IDeA) from the NIH/NIGMS P20GM103451 under the New Mexico IDeA Networks of Biomedical Research (NM-INBRE) Developmental Research Project Program (Mishra, PI of the Developmental Research Project).
Author information
Authors and Affiliations
Contributions
The study conception and design, obtaining funding, and providing leadership was performed by Shiraz Mishra. Material preparation and data collection were performed by Samantha Leekity, Joseph Rodman, Andrew Sussman, Keith Kelly, and Judith Sheche. Data analysis were performed by Prajakta Adsul, Joseph Rodman, and Andrew Sussman. The first draft of the manuscript was written by Shiraz Mishra and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no financial or non-financial competing interests.
Ethic approval
The UNM Health Sciences Center’s Human Research Review Committee (HRRC # 18–264) and the Southwest Tribal Institutional Review Board (SWT-2018–004) approved all aspects of the research protocol.
Consent to participate
All participants receive a consent letter and are informed about the research objectives and they voluntarily choose to participate. Further, they are informed that there is a very small risk of loss of privacy/confidentiality. Participants provide verbal consent to participate. Since the research poses no more than minimal risk of harm, the UNM Health Sciences Center’s Human Research Review Committee and the Southwest Tribal Institutional Review Board approved verbal consent for participation.
Consent to publish
Per the policies of the Tribe participating in the project, the Tribal leadership or its designees and the Tribal Institutional Review Board must consent for publication. In this instance, the Zuni Pueblo Tribal leadership and the Southwestern Tribal Institutional Review Board have agreed to publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mishra, S.I., Adsul, P., Leekity, S. et al. A culturally informed model to enhance breast, cervical, and colorectal cancer screenings: perspectives of American Indian adults and healthcare providers in rural New Mexico. Cancer Causes Control 34, 855–871 (2023). https://doi.org/10.1007/s10552-023-01721-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01721-y