Abstract
Purpose
To evaluate the impact of individual institutions on the outcome after surgery for Stanford type A aortic dissection (TAAD).
Methods
This is an observational, multicenter, retrospective cohort study including 3902 patients who underwent surgery for TAAD at 18 university and non-university hospitals.
Results
Logistic regression showed that four hospitals had increased risk of in-hospital mortality, while two hospitals were associated with decreased risk of in-hospital mortality. Risk-adjusted in-hospital mortality rates were lower in four hospitals and higher in other four hospitals compared to the overall in-hospital mortality rate (17.7%). Participating hospitals were classified as overperforming or underperforming if their risk-adjusted in-hospital mortality rate was lower or higher than the in-hospital mortality rate of the overall series, respectively. Propensity score matching yielded 1729 pairs of patients operated at over- or underperforming hospitals. Overperforming hospitals had a significantly lower in-hospital mortality (12.8% vs. 22.2%, p < 0.0001) along with decreased rate of stroke and/or global brain ischemia (16.5% vs. 19.9%, p = 0.009) compared to underperforming hospitals. Aggregate data meta-regression of the results of participating hospitals showed that hospital volume was inversely associated with in-hospital mortality (p = 0.043). Hospitals with an annual volume of less than 15 cases had an increased risk of in-hospital mortality (adjusted OR, 1.345, 95% CI 1.126–1.607).
Conclusion
The present findings indicate that there are significant differences between hospitals in terms of early outcome after surgery for TAAD. Low hospital volume may be a determinant of poor outcome of TAAD.
Trial registration
ClinicalTrials.gov Identifier: NCT04831073.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute Stanford type A aortic dissection (TAAD) is associated with high mortality [1]. Emergency surgical repair of TAAD is associated with early mortality rates higher than 10% and significant cerebral and visceral complications [2]. Interinstitutional differences may exist in terms of early and late outcome after surgery for TAAD, but only a few studies have evaluated this issue. Since, centralization of aortic surgery is advocated as a measure to improve the results of aortic surgery [3], more data are needed to support the creation of centers dedicated to the surgical and endovascular treatment of aortic diseases. We performed a multicenter, observational study on the outcome after surgery for acute TAAD and we hypothesized that differences in the outcome might exist between the participating centers. We evaluated this issue in the present analysis.
Methods
Study design
The present is an observational, multicenter, retrospective cohort study, which was approved by the Ethical Review Board of the Helsinki University Hospital, Finland (April 21, 2021, diary no. HUS/237/2021) and by the Ethical Review Board of each participating hospital. The requirement for informed consent was waived because of the retrospective nature of this study. The European Registry of Type A Aortic Dissection (ERTAAD) included consecutive patients who underwent surgery for acute TAAD at 18 centers of cardiac surgery located in eight European countries (Table 1) from January 1, 2005 to March 31, 2021. Data were retrospectively collected into a Microsoft Access datasheet (Redmond, Washington, USA) with pre-specified baseline, operative and outcome variables. Data on the date of death and repeated aortic intervention were collected retrospectively from electronic national registries as well as by contacting regional hospitals, patients and their relatives. Completeness of follow-up data varied significantly between centers and this was due to country-specific availability of methods to get data on follow-up.
Study participants
The study participants were recruited according to the following inclusion criteria: (1) TAAD or intramural hematoma involving the ascending aorta; (2) patients aged > 18 years; (3) symptoms started within 7 days prior to surgery; (4) primary surgical repair of acute TAAD; (5) any other major cardiac surgical procedure concomitant with surgery for TAAD [4]. The exclusion criteria were the following: (1) patients aged < 18 years; (2) onset of symptoms > 7 days prior to surgery; (3) prior procedure for TAAD; (4) retrograde TAAD (with primary tear located in the descending aorta); (5) concomitant endocarditis; (6) TAAD secondary to blunt or penetrating chest trauma [4].
Information regarding the definition criteria of risk factors have been previously reported [4]. Surgeon was defined experienced if had performed at least 20 elective or urgent procedures on the ascending aorta/aortic arch in the preceding year.
Outcome measures
The primary outcome of this study was in-hospital mortality, i.e., all-cause death occurred during the index hospitalization. The secondary outcomes were stroke, global brain ischemia, as well as a composite end-point including in-hospital mortality, stroke and global brain ischemia. Other secondary outcomes were need of mechanical circulatory support, dialysis, reoperation for intrathoracic bleeding, tracheostomy, mesenteric ischemia, 10-year rates of mortality as well as distal and proximal aortic reoperations. Definition criteria for these outcomes have been previously reported [4].
Statistical analysis
Categorical variables are reported as counts and percentages. Continuous variables are reported as means and standard deviations. Univariate analysis of continuous variables was performed using the Kruskal–Wallis’ test and of categorical variables using the Chi-square test. Survival analysis was performed using the Kaplan–Meier and competing risk analysis methods. Competing risk analyses using the Fine-Gray test with all-cause death as a competing event were performed to estimate difference between study groups in cumulative incidence of aortic reoperations. Logistic regression using the stepwise backward method was performed with the in-hospital mortality as the dependent variables and considering participating hospitals along with the following covariates associated with increased risk of in-hospital mortality: age, iatrogenic TAAD, preoperative cardiac massage, cerebral malperfusion, mesenteric malperfusion, peripheral malperfusion, aortic root replacement and aortic arch replacement and procedure performed by an experienced aortic surgeon. The risk-adjusted rate of in-hospital mortality was calculated by dividing, for each participating centre, the observed number of events by the expected number of events, and by multiplying this ratio by the average event rate of the entire series. The expected numbers of events were estimated using logistic regression. After plotting the risk-adjusted rates, participating hospitals were classified either as underperforming or overperforming if their risk-adjusted rate was higher or lower than the in-hospital mortality of the overall series, respectively. Considering the expected imbalance in the baseline and operative covariates, a propensity score matching analysis was performed employing a caliper width of 0.2 the standard deviation of the logit. Propensity score was calculated with logistic regression considering over- and under-performing hospitals as dependent variable and including all the covariates listed in Table 2, with the exception of aortic cross-clamping time and cardiopulmonary bypass time because they were expected to be part of the participating hospital’s characteristics. A standardized difference < 0.10 was considered as an acceptable balance between covariates of the study groups. The prognostic impact of hospital annual volume on in-hospital mortality was estimated using aggregated data meta-regression with random-effects. Furthermore, the median hospital volume of the participating hospitals was considered as a cutoff for high and low-volume hospitals and its effect was adjusted in multivariable logistic regression. Statistical analyses were performed with the SPSS (version 27.0, SPSS Inc., IBM, Chicago, Illinois, USA), Stata (version 15.1, StataCorp LLC, College Station, Texas, USA) and Open meta-analyst (version 2014, CESH, Brown University, Rhode Island, USA, cebm.brown.edu/openmeta/) statistical softwares.
Results
Participant characteristics
The mean age of patients was 63.3 (13.0) years, and there were 1185 (30.4%) females. DeBakey type I dissection was present in 3275 (83.8%) patients. TAAD was of iatrogenic origin in 103 (2.6%) of patients. The proportion of patients in the participating hospitals is summarized in Table 1. Participating hospitals significantly differed in terms of patients’ characteristics and operative approach (Table 2). Early and 10-year outcome differed between participating hospitals as well (Table 3).
In-hospital mortality
Overall, 689 (17.7%) patients died during the hospital stay (Table 3). Logistic regression including multiple covariates, as above listed, provided probabilities for hospital mortality whose area under the receiver operating characteristic curve was 0.687 (95% CI 0.664–0.709). Logistic regression confirmed that four hospitals (I, N, O, P) were associated with increased risk of in-hospital mortality, while two hospitals (S, T) were associated with decreased risk of in-hospital mortality. The other factors independently associated with in-hospital mortality are summarized in Table 4. It is worth noting that in this regression model, operation performed by experienced surgeon was not a factor associated with decreased risk of in-hospital mortality (p = 0.646).
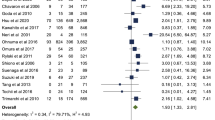
Risk-adjusted in-hospital mortality rates of each participating hospital are shown in Fig. 1. Risk-adjusted in-hospital mortality rates were lower in four hospitals and higher in other four hospitals compared to the overall in-hospital mortality rate (17.7%) (Fig. 1).
Risk-adjusted rates with 95% confidence intervals of in-hospital mortality after surgery for acute type A aortic dissection at the participating hospitals. Red line is the rate of in-hospital mortality in the overall series, red dots indicate hospitals with significantly higher risk-adjusted rates and green dots indicate hospitals with significantly lower risk-adjusted rates
Propensity score matching analysis
Participating hospitals were classified as overperforming or underperforming if their risk-adjusted in-hospital mortality rate was lower or higher than the in-hospital mortality rate of the overall series, respectively (Fig. 1). Based on this criterion, nine hospitals were classified as overperforming and nine hospitals as underperforming. Propensity score matching with a caliper of 1.4 yielded 1729 pairs with comparable baseline and operative covariates (Table 5). Among propensity score matched cohorts, overperforming hospitals had a significantly lower in-hospital mortality (12.8% vs. 22.2%, p < 0.0001) along with decreased rate of stroke and/or global brain ischemia (16.5% vs. 19.9%, p = 0.009) and mesenteric ischemia (2.5% vs. 5.0%, p < 0.0001) (Table 6). Overperforming hospitals had increased rate of re-exploration for intrathoracic bleeding (15.5% vs. 12.8%, p = 0.025). A 10-year, patients operated in overperforming hospitals had lower mortality (45.0% vs. 49.8%, p < 0.0001) (Fig. 2), but higher rate of distal aortic reoperation (9.8% vs. 5.2%, p < 0.0001). A trend toward increased risk of proximal aortic reoperation was observed in patients operated in overperforming hospitals (5.2% vs. 3.3%, p = 0.051).
Impact of hospital volume on in-hospital mortality
Aggregate meta-regression of the results of participating hospitals showed that hospital volume was inversely associated with in-hospital mortality (omnibus p = 0.043, intercept coefficient 0.244, 95% CI 0.177–0.311) (Fig. 3). The median hospital volume (14 cases/year) was considered as a cutoff for high-volume hospitals (9) and low-volume hospitals (9) and its effect was significant in aggregate data meta-regression. Furthermore, hospitals with an annual volume < 15 cases/year had an increased risk of in-hospital mortality in multivariable logistic regression (adjusted OR, 1.345, 95% CI 1.126–1.607).
Discussion
The findings of the present study can be summarized as follows: (1) the early outcome of surgery for TAAD may significantly differ between hospitals; (2) low hospital volume of surgical procedure for TAAD may be a determinant of poor outcome.
The main aim of this study was to identify outlier hospitals in terms of perioperative mortality. We were able to identify four centers whose results seemed unsatisfactory compared to the other hospitals in terms of average in-hospital mortality. Furthermore, the estimation of risk-adjusted mortality rates allowed us to classify hospitals as under- or over-performing and propensity score matching prevented any imbalance in baseline and operative covariates inasmuch that these might potentially have affected the results. Indeed, we observed that overperforming hospitals performed more frequently aortic root and aortic arch replacement procedures and, despite this, their outcome was more favorable. Meta-regression showed that low volume of surgery for TAAD may explain such differences as it was confirmed by adjusted regression analysis. We observed that also 10-year mortality was lower in patients operated in overperforming hospital, but this seems mainly an effect of the initial lower early mortality. Overperforming hospitals had increased rates of late aortic reoperation. We hypothesize that these centers might have larger experience in aortic procedures, closer follow-up and had a more active policy of repair of aortic dissection-related complications also on the long run. However, the proportion of reoperation was rather low in both groups.
Regarding the impact of hospital volume on the outcome of surgery for TAAD, three large studies have previously investigated this issue. Kazui et al. [5] reported on a mortality of 16.3% in 10,097 TAAD patients operated on at 439 Japanese institutions from 2000 to 2004. In their series, only four hospitals had an annual volume of TAAD surgery of ≥ 20 cases and their mortality was 7.9%. Hospitals with annual volume < 5 cases had a mortality of 18.5% (OR 2.16, 95% CI 1.48–3.16). The difference between the high-volume and low-volume centers was statistically significant.
Brescia et al. [6] evaluated the outcome of 2918 patients who underwent surgery for TAAD patients operated at 232 hospitals from 2010 to 2014 in seven countries of the United States. The in-hospital mortality was 15.9% and was dependent on the hospital volume. The in-hospital mortality rate 20.8% in hospitals with of < 3 annual cases, 16.7% with 3–5 annual cases, 14.9% for 6–10 annual cases and 11.5% for more than 10 annual cases (p < 0.001).
Dobaria et al. [7] reported the results of 25,231 patients from the National Inpatient Sample (NIS) operated for TAAD between 2005 and 2014. Hospitals were classified as low-, medium- and high-volume based on tertiles of their open-thoracic aortic operative caseload and showed in hospital mortality of 21.5%, 16.8% and 11.6%, respectively (p < 0.001). Neurological complications were reported in 15.2%, 11.9% and 11.5%, respectively (p = 0.002). Importantly, the rates of overall complications were rather high, but they did not differ between the study groups (p = 0.11). This study provided the benefits of analyzing their results based on the aortic surgery caseload rather than the TAAD caseload. The former caseload may be a more reliable measure of the surgical and anesthesiological expertise than the less frequently encountered TAAD. Interestingly, the overall complication rates were similar between the study groups, still in-hospital mortality was significantly lower among high-volume hospitals. Such findings were observed also in the propensity score matched cohorts of this study. These findings suggest that, despite a high incidence of postoperative complications, overperforming hospitals can provide a better perioperative care for these complications than underperforming centers.
Consonant with these results, Mariscalco et al. [3] reported the results of a pooled analysis on 30 studies on acute aortic syndrome and showed that high-volume centers were associated with significantly lower mortality (OR 0.51, 95% CI 0.46–0.56). These authors demonstrated also that high-volume surgeons decreased the risk of mortality as well (OR 0.41, 95% CI 0.25–0.66). The findings are similar to those observed after surgery for ruptured abdominal aortic aneurysm, in which hospital volume, but not surgeon’s volume, had a significant impact on perioperative mortality [8].
The retrospective nature is the main limitation of this study. Second, we do not have data on individual surgeon’s volume. Despite the relatively large size of this database, this would not have allowed a reliable analysis of this important issue because the number of procedures for TAAD per surgeons might still have been rather small. Third, no data were available on the proportion and outcome of patients who were not treated for aortic-related complications. Finally, participating hospitals might have differed significantly for referral pathway and distance from patient’s residence. This means that hospitals might have a lower caseload because referral of patients is slower as several patients might have died during transportation. Similarly, long distances may be associated with worse clinical conditions, which cannot be stratified only by clinical variables.
In conclusion, the present findings indicate that there are significant differences between hospitals in terms of early outcome after surgery for TAAD. Low hospital volume of TAAD may be a determinant of poor outcome in these patients.
References
Benedetto U, Dimagli A, Kaura A, et al. Determinants of outcomes following surgery for type A acute aortic dissection: the UK National Adult Cardiac Surgical Audit. Eur Heart J. 2021;43:44–52. https://doi.org/10.1093/eurheartj/ehab586.
Larsen M, Trimarchi S, Patel HJ, et al. Extended versus limited arch replacement in acute Type A aortic dissection. Eur J Cardiothorac Surg. 2017;52:1104–10. https://doi.org/10.1093/ejcts/ezx214.
Mariscalco G, Maselli D, Zanobini M, et al. Aortic centres should represent the standard of care for acute aortic syndrome. Eur J Prev Cardiol. 2018;25(1_suppl):3–14. https://doi.org/10.1177/2047487318764963.
Biancari F, Mariscalco G, Yusuff H, et al. European registry of type A aortic dissection (ERTAAD)—rationale, design and definition criteria. J Cardiothorac Surg. 2021;16(1):171. https://doi.org/10.1186/s13019-021-01536-5.
Brescia AA, Patel HJ, Likosky DS, et al. Volume-outcome relationships in surgical and endovascular repair of aortic dissection. Ann Thorac Surg. 2019;108:1299–306. https://doi.org/10.1016/j.athoracsur.2019.06.047.
Kazui T, Osada H, Fujita H. An attempt to analyze the relation between hospital surgical volume and clinical outcome. Gen Thorac Cardiovasc Surg. 2007;55:483–92. https://doi.org/10.1007/s11748-007-0172-0.
Dobaria V, Kwon OJ, Hadaya J, et al. Impact of center volume on outcomes of surgical repair for type A acute aortic dissections. Surgery. 2020;168:185–92. https://doi.org/10.1016/j.surg.2020.04.007.
Kontopodis N, Galanakis N, Akoumianakis E, Ioannou CV, Tsetis D, Antoniou GA. Systematic review and meta-analysis of the impact of institutional and surgeon procedure volume on outcomes after ruptured abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2021;62:388–98. https://doi.org/10.1016/j.ejvs.2021.06.015.
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital. This study was not funded or supported financially.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No disclosures were reported by the coauthors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biancari, F., Dell’Aquila, A.M., Gatti, G. et al. Interinstitutional analysis of the outcome after surgery for type A aortic dissection. Eur J Trauma Emerg Surg 49, 1791–1801 (2023). https://doi.org/10.1007/s00068-023-02248-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02248-2