Abstract
PaO2/FiO2 (P/F ratio) is considered a marker of hypoxia/hypoxemia and mortality. Several prothrombotic changes are associated with the decrease of P/F ratio. The role of P/F ratio in patients with arterial and venous thrombosis remains unclear. The aim of this study was to assess in patients with coronavirus disease 2019 (COVID-19), the association between P/F ratio and arterial/venous thrombosis. One thousand and four hundred and six COVID-19 patients were recruited; 289 (21%) patients had P/F ratio < 200 and 1117 (79%) ≥ 200. Compared to the patients with P/F ratio ≥ 200, those with P/F ratio < 200 were older and with higher levels of glycemia, D–dimer and lower levels of albumin. Multiple linear regression analysis showed that albumin (standardized coefficient β: 0.156; SE: 0.001; p = 0.0001) and D–dimer (standardized coefficient β: -0.135; SE: 0.0001; p = 0.0001) were associated with P/F ratio. During the hospitalization 159 patients were transferred in intensive care unit (ICU), 253 patients died, 156 patients had arterial or venous thrombotic events. A bivariate logistic analysis was performed to analyze the predictors of thrombosis in COVID-19 patients; P/F ratio < 200 (Odds Ratio: [OR] 1.718, 95% Confidence Interval [CI] 1.085–2.718, p = 0.021), albumin (OR 1.693, 95% CI 1.055–2.716, p = 0.029), D-dimer (OR 3.469, 95% CI 2.110–5.703, p < 0.0001), coronary artery disease (CAD) (OR 1.800, 95% CI 1.086–2.984, p = 0.023) and heart failure (OR 2.410 95% CI 1.385–4.193, p = 0.002) independently predicted thrombotic events in this population. This study suggests that the P/F ratio is associated with thrombotic events by promoting a hypercoagulation state in patients hospitalized for COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 is a pandemic associated with increased risk in the development of arterial and venous thrombotic events and death [1, 2]. The risk factors associated with the increased thrombotic risk are still unclear. Since COVID-19 is a disease that can cause pneumonia and therefore seriously affecting the respiratory function, some studies analyzed the role of the PaO2/FiO2 ratio (P/F ratio) and its impact on clinical outcome. P/F ratio is the ratio between arterial partial pressure of oxygen (PaO2) and fraction of inspired oxygen (FiO2) and is a marker of systemic hypoxia. It is currently used as a marker of acute respiratory failure in COVID-19 patients [3] and in adult patients with acute respiratory distress syndrome (ARDS) [4]. A P/F < 200 is considered a cutoff associated with a serious risk of developing ARDS and respiratory failure [5].
Several previous studies showed that a low P/F ratio is associated with a higher risk of mortality [3, 6] but there is scarce evidence of its association with thrombotic events in COVID-19 patients. However, it is arguable that the P/F ratio could be associated with thrombosis as animal and human studies have shown that hypoxia is strongly associated with thrombosis through mechanisms that activate platelets, increase levels of tissue factor, clotting factors or impair fibrinolysis [7].
For its simplicity, rapidity of execution and low cost the P/F ratio could represent a valid instrument to stratify the risk of developing thrombotic events in patients affected by COVID-19. Thus, in this study we want to assess if P/F ratio is associated with arterial and venous thrombotic events in COVID-19 patients.
Materials and methods
Study design and population
This is an observational retrospective cohort multi-center study performed in Italian Hospitals devoted to COVID-19 care. This study was performed in non-intensive care unit (ICU) medical wards. We enrolled consecutive patients, according to the inclusion/exclusion criteria form cohort from Rome Hospitals and from Aquila, Chieti, Latina, Perugia, Avellino and Viterbo.
We included in the study adult (≥ 18 years) patients with laboratory-confirmed COVID-19 and acute respiratory syndrome coronavirus-2 (SARS-CoV2)-related pneumonia which needed hospitalization, requiring or not mechanical ventilation, consecutively admitted to Medicine wards from March 2020 to March 2021. COVID-19 was diagnosed on the basis of the WHO interim guidance [8]. COVID-19 pneumonia was diagnosed by chest computed tomography. A COVID-19 case was defined as a person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms. Each hospital involved in this study recorded COVID-19 cases and forwarded the data to the national health ministry. During the intra-hospital stay any vascular event was registered. Demographic and clinical characteristics were collected after receiving informed consent. Routine analysis included P/F ratio, D-dimer and albumin executed within 48 h from the admission at the hospital. Ethical approval for this study was obtained from Ethics Committee of Azienda Ospedaliero Universitaria Policlinico Umberto I (ID Prot. 109/2020).
Baseline assessment
Demographic and anamnestic characteristics, along with baseline clinical, laboratory and radiological results were extracted from electronic medical records of patients enrolled. Data regarding demographic characteristics, comorbidities, and concurrent therapy were collected. Pre-existence of diabetes mellitus, hypertension, cardiovascular disease, chronic kidney disease, and obesity were defined as previously described [9].
Primary end-points
Arterial and venous thrombosis occurring during the hospitalization were the primary end-point of the study. The appearance of new ischemic/embolic events was diagnosed as follows: (1) pulmonary thromboembolism by lung CT scan; [10] (2) myocardial infarction by EKG changes associated with enhanced markers of cell necrosis; [11] (3) acute brain ischemia by onset of new focal neurological signs and symptoms and confirmed, whenever possible, by NMR or CT imaging; [12] (4) deep venous thrombosis in symptomatic patients was diagnosed by compression ultrasonography [13,14,15].
Fatal myocardial infarction was defined as previously described by the World Health Organization [16]. Microembolization of the clots originated in the heart or other arterial districts distant to the artery lower limbs responsible of arterial occlusion and ischemia where diagnosed as previously described [17].
Statistical analysis
Data are expressed as mean and standard deviation (SD) or median and interquartile range (IQR) according to their distribution for continuous variables, and count and percentages for categorical ones.
Comparison between groups was performed by Chi square test, Student T test, or Mann–Whitney test as appropriate. Bivariate analysis was performed by Pearson's Correlation Coefficient. The variables with evidence of an association p < 0.10 were included in a multivariable linear regression using an automated procedure with forward selection. The results of the multivariable linear regression analysis were expressed as standardized coefficient beta (β) with standard error (SE), moreover the coefficient of determination was provided (R2). A p value of < 0.05 was considered statistically significant. A multivariable logistic regression model was estimated, and the odds-ratios obtained were used to derive weighting factors of thrombosis. We used the following cut-offs for D–dimer and albumin: D–dimer ≥ 1100 ng/mL and albumin < 35 g/L for chi-square and logistic regression analysis, while we treated them as continuous variables in bivariate correlation and multiple linear regression analysis.
All tests were two-tailed, and a value of p < 0.05 was considered as statistically significant. Analyses were performed using IBM SPSS statistic version 25.
Results
One thousand and four hundred and six COVID-19 patients were recruited; 289 (21%) patients had P/F ratio < 200 and 1117 (79%) ≥ 200. The mean period of hospitalization was 19 ± 18 days. At admission, two hundred and one patients were already treated with anticoagulants.
Compared to the patients with P/F ratio ≥ 200, those with P/F ratio < 200 were older, with a major need of intensive care unit (ICU) and with a higher prevalence of smoking, coronary artery disease (CAD), thrombotic events and dementia (Table 1). Furthermore, they have higher levels of glycemia, D–dimer, IMPROVEDD score and lower albumin. Finally, patients with P/F < 200 ratio had a significant higher prevalence of steroids and heparins low-molecular-weight heparins (LMWH) use (Table 1).
Bivariate correlation analysis showed that P/F ratio correlated with serum albumin (R: 0.227, p < 0.0001), D-Dimer (R: − 0.240 p < 0.0001), age (R: − 0.347, p < 0.0001), SpO2 (R: 0.258, p < 0.0001) in the overall population; no correlation was observed between P/F ratio and serum creatinine (R: − 0.022, p = 0.476). A significant inverse correlation was detected between D-dimer and serum albumin (R: − 0.206, p < 0.0001).
Multiple linear regression analysis showed that albumin (standardized coefficient β: 0.156; SE: 0.001; p = 0.0001), D-dimer (standardized coefficient β: -0.135; SE: 0.0001; p = 0.0001), were the independent predictive variables associated with P/F ratio (R2 = 30%).
During the hospitalization 159 patients were transferred in ICU, 253 patients died, 156 patients had the following thrombotic events: micro-embolism n = 5 (3%), deep venous thrombosis n = 42 (27%), pulmonary embolism n = 36 (23%), peripheral artery ischemia n = 9 (6%), myocardial infarction n = 36 (23%), transient ischemic attack (TIA)/stroke n = 28 (18%) (Table 2).
Table 2 reports the clinical characteristics and treatment of patients with and without thrombotic events occurred during hospitalization. Compared to the patients who did not experience thrombotic events, patients with thrombotic events were older, with an higher prevalence of former smokers, hypertension, atrial fibrillation, coronary artery disease (CAD), heart failure, peripheral vascular disease, TIA/stroke, COPD, and a higher need of intensive care unit (ICU). Furthermore, they had higher IMPROVEDD Score, creatinine, D–dimer, and lower P/F ratio and albumin. Furthermore, they have a significant higher prevalence of steroids and heparins low-molecular-weight heparins (LMWH) use (Table 2).
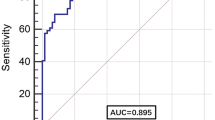
A bivariate logistic analysis was performed to analyze the predictors of thrombosis in COVID-19 patients; P/F ratio < 200 (OR 1.718, 95% CI 1.085–2.718, p = 0.021), albumin (OR 1.693, 95% CI 1.055–2.716, p = 0.029), D-dimer (OR 3.469, 95% CI 2.110–5.703, p < 0.0001), CAD (OR 1.800, 95% CI 1.086–2.984, p = 0.023) and heart failure (OR 2410, 95% CI 1.385–4.193, p = 0.002) independently predicted thrombotic events in this population (see Table 3).
Discussion
The present study shows that patients affected by COVID-19 with P/F ratio < 200 have a high risk to develop arterial and venous thrombotic events.
To the best of our knowledge, only an Italian single-center study reported a significant association between P/F ratio and thrombosis in a limited number of COVID-19 patients (n = 180) [18], but the interplay between P/F ratio and mechanisms of thrombosis was not investigated. The novelty of the present study is the relationship between P/F ratio and D–dimer suggesting that hypoxia may be a trigger of clotting activation. This hypothesis is in keeping with previous reports showing that hypoxemia may generate arterial and venous thrombosis [7, 19]. Thus, observational and experimental studies showed that hypoxia/hypoxemia increased the risk of thrombosis [7, 19]. Virchow’s triad (hypercoagulability, endothelial injury and stasis) seems to be implicated in this physio-pathological process [7]. Local and systemic hypoxia due to several risk factors (as cancer, high altitude, immobilization after major trauma or surgical interventions, etc.) activate the hypoxia-inducible transcription factors (HIFs) that regulate the genes that mediate coagulation and fibrinolysis [7, 19]. Thus, the HIFs activation leads to the increase of prothrombotic substances as tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6, IL-12, plasminogen activator inhibitor (PAI)-1 [7] or to decrease anticoagulant factors as protein S [20]. All this pathological process is well summed up by some animal studies that have shown how hypoxia increases the incidence of experimental venous thrombosis in mice [7, 21].
Hypoxia is also implicated in thrombosis of the arterial district. Experimental studies in patients with peripheral arterial disease showed that when platelets are exposed to hypoxia, platelet activation proteins, P-selectin, fibrinogen binding protein expression and GpIIb/IIIa will increase [7, 22] favoring a prothrombotic state. In addition, hypoxia causes vasoconstriction favoring the formation of micro thrombosis and decreasing the share of pulmonary perfusion [23].
The association between P/F ratio and albumin is another novel finding that may provide new insight into the relationship between P/F ratio and thrombosis in COVID-19. We have previously demonstrated the prothrombotic role of serum albumin and D–dimer in patients with COVID-19 [24, 25] and that restoring serum albumin levels improves the thrombotic risk in this setting [25]. Thus, albumin is implicated in both clotting and platelet activation with several mechanisms such as inhibition of fibrin polymerization, increase of the antithrombin III action, and modulating the hepatic synthesis of factor V, factor VIII, and fibrinogen [26, 27]. Furthermore, albumin impairs platelet aggregation downregulating Nox2 activation, a powerful source of reactive oxidant species [28].
At this regard, it is also interesting to note that the administration of albumin before a lung transplant, administered to improve the prothrombotic state, is able to increase the P/F ratio [29]. It remains to be established, however, the association between hypoxia and albumin. Low serum albumin levels could contribute to pulmonary edema formation and to consequent hypoxia in patients with ARDS [30]. Furthermore, a previous study in hypo-proteinemic patients with ARDS showed that those treated with albumin had an increase of oxygenation as assessed by P/F ratio [31].
In accordance with previous studies, we found an association among coronary heart disease (CAD), heart failure and cardiovascular events in patients with COVID [32]. Patients affected by CAD and heart failure are more inclined to have arterial and venous thrombotic events and mortality after pneumonia [33, 34]. Increased platelet aggregation and clotting system activation, as documented by up-regulation of tissue factor and down-regulation of activated protein C, could be implicated in this process [33, 34].
The study has limitations. We reported the P/F ratio assessed at admission in the medical wards thus, this parameter could change during hospitalization. We did not stratify the population according to the COVID-19 waves therefore, different incidences of thrombosis could be present according different periods of hospitalization.
In conclusion, the study shows that P/F ratio is associated to thrombotic events in patients hospitalized for COVID-19 and suggests hypoalbuminemia as a mechanism accounting for hypoxia-related hypercoagulability.
Data availability
Data will be available upon reasonable request to the corresponding author.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CAD:
-
Coronary artery disease
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- CT:
-
Computer tomography
- EKG:
-
Electrocardiogram
- FiO2:
-
Fraction of inspired oxygen
- HIFs:
-
Hypoxia-inducible transcription factors
- ICU:
-
Intensive care unit
- IL:
-
Interleukin
- LMWH:
-
Low molecular weight heparin
- NMR:
-
Nuclear magnetic resonance
- PAI:
-
Plasminogen activator inhibitor
- PaO2:
-
Arterial partial pressure of oxygen
- PaO2/FiO2 :
-
P/F ratio
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- TIA:
-
Transient ischemic attack
- TNF:
-
Tumor necrosis factor
References
Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo L (2020) Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost 120(6):949–956. https://doi.org/10.1055/s-0040-1710317
Loffredo L, Di Castelnuovo A, Chiariello GA, Pignatelli P, Violi F (2022) Full versus prophylactic-intermediate doses of anticoagulants in COVID-19: a meta-analysis. Haematologica 107(8):1933–1939. https://doi.org/10.3324/haematol.2022.280652
Prediletto I, D’Antoni L, Carbonara P, Daniele F, Dongilli R, Flore R et al (2021) Standardizing PaO2 for PaCO2 in P/F ratio predicts in-hospital mortality in acute respiratory failure due to Covid-19: a pilot prospective study. Eur J Intern Med 92:48–54. https://doi.org/10.1016/j.ejim.2021.06.002
Griffiths MJD, McAuley DF, Perkins GD, Barrett N, Blackwood B, Boyle A et al (2019) Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res 6(1):000420. https://doi.org/10.1136/bmjresp-2019-000420
Suchyta MR, Orme JF Jr, Morris AH (2003) The changing face of organ failure in ARDS. Chest 124(5):1871–1879. https://doi.org/10.1378/chest.124.5.1871
Gu Y, Wang D, Chen C, Lu W, Liu H, Lv T et al (2021) PaO2/FiO2 and IL-6 are risk factors of mortality for intensive care COVID-19 patients. Sci Rep 11(1):7334. https://doi.org/10.1038/s41598-021-86676-3
Gupta N, Zhao YY, Evans CE (2019) The stimulation of thrombosis by hypoxia. Thromb Res 181:77–83. https://doi.org/10.1016/j.thromres.2019.07.013
World Health Organization (2020) Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. Pediatr Med Rodz 16:9–26
Cangemi R, Casciaro M, Rossi E, Calvieri C, Bucci T, Calabrese CM et al (2014) Platelet activation is associated with myocardial infarction in patients with pneumonia. J Am Coll Cardiol 64(18):1917–1925. https://doi.org/10.1016/j.jacc.2014.07.985
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP et al (2019) ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The task force for the diagnosis and management of acute pulmonary embolism of the European society of cardiology (ESC). Eur Respir J. https://doi.org/10.1183/13993003.01647-2019
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA et al (2018) Fourth universal definition of myocardial infarction (2018). Circulation 138(20):e618–e651. https://doi.org/10.1161/CIR.0000000000000617
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the american heart association/American stroke association. Stroke 50(12):e344–e418. https://doi.org/10.1161/STR.0000000000000211
Loffredo L, Arienti V, Vidili G, Cogliati C, Battaglia S, Perri L et al (2019) Low rate of intrahospital deep venous thrombosis in acutely Ill medical patients: results from the AURELIO study. Mayo Clin Proc 94(1):37–43. https://doi.org/10.1016/j.mayocp.2018.07.020
Needleman L, Cronan JJ, Lilly MP, Merli GJ, Adhikari S, Hertzberg BS et al (2018) Ultrasound for lower extremity deep venous thrombosis: multidisciplinary recommendations from the society of radiologists in ultrasound consensus conference. Circulation 137(14):1505–1515. https://doi.org/10.1161/CIRCULATIONAHA.117.030687
Loffredo L, Vidili G, Sciacqua A, Cogliati C, Di Giulio R, Bernardini S et al (2022) Asymptomatic and symptomatic deep venous thrombosis in hospitalized acutely ill medical patients: risk factors and therapeutic implications. Thromb J 20(1):72. https://doi.org/10.1186/s12959-022-00433-8
Mendis S, Thygesen K, Kuulasmaa K, Giampaoli S, Mahonen M, Ngu Blackett K et al (2011) World health organization definition of myocardial infarction: 2008–09 revision. Int J Epidemiol 40(1):139–146. https://doi.org/10.1093/ije/dyq165
Lyaker MR, Tulman DB, Dimitrova GT, Pin RH, Papadimos TJ (2013) Arterial embolism. Int J Crit Illn Inj Sci 3(1):77–87. https://doi.org/10.4103/2229-5151.109429
Ramirez GA, Calvisi SL, de Lorenzo R, da Prat V, Borio G, Gallina G et al (2021) A novel evidence-based algorithm to predict thromboembolism in patients with COVID-19: preliminary data from a single-centre cohort. Minerva Med. https://doi.org/10.23736/S0026-4806.21.07331-6
Yan SF, Mackman N, Kisiel W, Stern DM, Pinsky DJ (1999) Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler Thromb Vasc Biol 19(9):2029–2035. https://doi.org/10.1161/01.atv.19.9.2029
Pilli VS, Datta A, Afreen S, Catalano D, Szabo G, Majumder R (2018) Hypoxia downregulates protein S expression. Blood 132(4):452–455. https://doi.org/10.1182/blood-2018-04-841585
Brill A, Suidan GL, Wagner DD (2013) Hypoxia, such as encountered at high altitude, promotes deep vein thrombosis in mice. J Thromb Haemost 11(9):1773–1775. https://doi.org/10.1111/jth.12310
Cameron SJ, Mix DS, Ture SK, Schmidt RA, Mohan A, Pariser D et al (2018) Hypoxia and ischemia promote a maladaptive platelet phenotype. Arterioscler Thromb Vasc Biol 38(7):1594–1606. https://doi.org/10.1161/ATVBAHA.118.311186
Habashi NM, Camporota L, Gatto LA, Nieman G (2021) Functional pathophysiology of SARS-CoV-2-induced acute lung injury and clinical implications. J Appl Physiol 130(3):877–891. https://doi.org/10.1152/japplphysiol.00742.2020
Violi F, Pignatelli P, Vestri AR, Spagnoli A, Cipollone F, Ceccarelli G et al (2022) The ADA (Age-D-Dimer-Albumin) score to predict thrombosis in SARS-CoV-2. Thromb Haemost 122(9):1567–1572. https://doi.org/10.1055/a-1788-7592
Violi F, Ceccarelli G, Loffredo L, Alessandri F, Cipollone F, D’Ardes D et al (2021) Albumin supplementation dampens hypercoagulability in Covid-19: a preliminary report. Thromb Haemost 121(1):102–105. https://doi.org/10.1055/s-0040-1721486
Galanakis DK (1992) Anticoagulant albumin fragments that bind to fibrinogen/fibrin: possible implications. Semin Thromb Hemost 18(1):44–52. https://doi.org/10.1055/s-2007-1002409
Mikhailidis DP, Ganotakis ES (1996) Plasma albumin and platelet function: relevance to atherogenesis and thrombosis. Platelets 7(3):125–137. https://doi.org/10.3109/09537109609023571
Basili S, Carnevale R, Nocella C, Bartimoccia S, Raparelli V, Talerico G et al (2019) Serum albumin is inversely associated with portal vein thrombosis in cirrhosis. Hepatol Commun 3(4):504–512. https://doi.org/10.1002/hep4.1317
Vajter JDM (2022) Volume replacement strategy with albumin 5% and bedside coagulopathy management improves cardiopulmonary stability by decreasing norepinephrine dosage and by increasing P/F ratio in patients undergoing lung transplantation (preliminary results). J Heart Lung Transplant 38(4):821. https://doi.org/10.1016/j.healun.2019.01.831
McNeil JB, Jackson KE, Wang C, Siew ED, Vincz AJ, Shaver CM et al (2021) Linear association between hypoalbuminemia and increased risk of acute respiratory distress syndrome in critically ill adults. Crit Care Explor 3(9):e0527. https://doi.org/10.1097/CCE.0000000000000527
Uhlig C, Silva PL, Deckert S, Schmitt J, de Abreu MG (2014) Albumin versus crystalloid solutions in patients with the acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care 18(1):R10. https://doi.org/10.1186/cc13187
Violi F, Ceccarelli G, Cangemi R, Cipollone F, D’Ardes D, Oliva A et al (2021) Arterial and venous thrombosis in coronavirus 2019 disease (Covid-19): relationship with mortality. Intern Emerg Med 16(5):1231–1237. https://doi.org/10.1007/s11739-020-02621-8
Violi F, Cangemi R, Calvieri C (2014) Pneumonia, thrombosis and vascular disease. J Thromb Haemost 12(9):1391–1400. https://doi.org/10.1111/jth.12646
Violi F, Cangemi R, Falcone M, Taliani G, Pieralli F, Vannucchi V et al (2017) Cardiovascular complications and short-term mortality risk in community-acquired pneumonia. Clin Infect Dis 64(11):1486–1493. https://doi.org/10.1093/cid/cix164
Acknowledgements
Unit of Anaesthesia, Intensive Care and Pain Management, Department of Medicine, Università Campus Bio-Medico di Roma, Rome, Italy: Fausto D'Agostino, Felice Eugenio Agrò, Alessia Mattei; Internal Medicine Unit, Moscati Hospital, Avellino, Italy: Loredana Tibullo, Maria Grazia Nunziata, Valeria Iorio, Natalia Iuliano, Sara Mangiacapra, Mariangela Raimondo, Mariangela Atteno; Clinica Medica, Department of Medicine and Aging, “G. D’Annunzio, University of Chieti-Pescara, Chieti, Italy: Claudio Ferri, Davide Grassi, Giovambattista Desideri, Stefano Abballe; Mediterranea Cardiocentro-Napoli, Via Orazio, 2, 80122 Napoli, Italy: Claudio Ferri, Davide Grassi, Giovambattista Desideri, Stefano Abballe; Protect Medicine Division, Belcolle Hospital, Viterbo, Italy: Serena Dell'Isola; Dipartimento Emergenza E Accettazione, Ospedale Universitario Sant'Andrea, Rome, Italy: Monica Rocco, Daniela Alampi; SM Goretti Hospital, Latina, Italy: Cosmo Del Borgo; Department of Maternal Sciences, Sapienza University of Rome, Italy Viale Regina Elena, 324 00161, Rome, Italy: Vanessa Bianconi, Massimo Raffaele Mannarino, Filippo Figorilli; Department of Clinical Internal, Anesthesiologic and Cardiovascular Sciences, Sapienza University of Rome, Viale del Policlinico, 155, 00161 Rome: Alessia Fallarino, Ilaria Maria Palumbo, Arianna Pannunzio, Arianna Magna, Chiara Bagnato, Alba Rosa Alfano
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. No support has been received for this study.
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: LL. Acquisition, analysis, or interpretation of data: PP, GC, AO, FT, CQ, EM, VB, MRM, FF, EC, FP, EE, MV, AZ, BC, CMM. Drafting of the manuscript: FV and LL. Critical revision of the manuscript for important intellectual content: PP, EE. Statistical analysis: EM, LL. Study supervision: FV.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflicts of interest concerning this paper.
Ethical approval
The present research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Human and animal rights
Ethical approval for this study was in accordance with the Declaration of Helsinki for human and animal rights.
Informed consent
Patient consent was waived due to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the COVID group are listed in acknowledgements.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Loffredo, L., Pignatelli, P., Pirro, M. et al. Association between PaO2/FiO2 ratio and thrombotic events in COVID-19 patients. Intern Emerg Med 18, 889–895 (2023). https://doi.org/10.1007/s11739-023-03196-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03196-w