Abstract
Background and Objective
Palovarotene, a selective retinoic acid receptor γ agonist, is under investigation for the treatment of dry eye disease. This study aimed to determine the ocular and systemic safety, tolerability and pharmacokinetics of palovarotene ophthalmic solution (PVO-OS) in healthy adults.
Methods
This was a randomised, vehicle-controlled phase I study (NCT04762355; retrospectively registered). Participants received either PVO-OS (at 0.025, 0.05 or 0.10 mg/mL) or a vehicle (placebo-to-match PVO-OS) once-daily or twice-daily for seven consecutive days. Safety was assessed by ocular and systemic assessments. Blood samples for pharmacokinetic assessments were collected before and after dose administration.
Results
Thirty-six participants were randomised to PVO-OS and 12 to the vehicle. Overall, 89 treatment-emergent ocular adverse events (TEOAEs) were reported by 22 participants (61.1%) receiving PVO-OS and ten TEOAEs were reported by five participants (41.7%) receiving the vehicle. Erythema, irritation and skin dryness of the eyelid were the most common TEOAEs in participants receiving PVO-OS. The incidence of TEOAEs and eyelid-related findings in the PVO-OS groups increased with ascending dose and frequency compared with participants treated with the vehicle. All TEOAEs were mild (96.6%) or moderate (3.4%) and resolved without sequelae. Plasma palovarotene concentrations were generally measurable for up to 3–4 h for 0.025 mg/mL and 0.05 mg/mL and up to 12 h for 0.10 mg/mL dose regimens, independent of the frequency of administration.
Conclusions
PVO-OS was generally well tolerated at doses up to and including 0.10 mg/mL twice daily. Similar pharmacokinetic profiles were observed for the once-daily and twice-daily regimens following multiple ascending doses of PVO-OS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A novel ophthalmic solution is under investigation for the treatment of dry eye disease. Doses up to and including 0.10 mg/mL received twice daily were generally well tolerated. There were no serious adverse events. |
1 Introduction
Dry eye disease (DED) is a disorder of the ocular surface characterised by a loss of homeostasis of the tear film [1]. The most common clinical symptoms of DED include ocular burning and stinging, photophobia and blurred vision. These symptoms can impact visual function and reduce quality of life (QoL) in patients with DED [2]. Owing to the lack of a standardised worldwide definition, the global prevalence of DED is estimated to be between 5 and 50%; prevalence increases significantly with age and is greater in women [1, 3].
Current treatment for DED involves a stepped approach corresponding to disease severity, with artificial tears the mainstay of therapy [3, 4]. Because of the inflammatory nature of DED, topical nonsteroidal anti-inflammatory medications, tetracyclines and corticosteroids are common next-line therapies [5, 6]. Until the recent US Food and Drug Administration approval of loteprednol etabonate ophthalmic suspension (0.25%) [7], cyclosporine and lifitegrast were the only prescription medications approved by the Food and Drug Administration to alleviate the signs and symptoms of DED [8]. Of these, only a cyclosporine 1 mg/mL emulsion is approved for the treatment of DED in Europe [9]. However, cyclosporine and lifitegrast have limited efficacy and a slow onset for some patients [10, 11]. Ocular burning is a common side effect of topical cyclosporine (occurring in up to 17% of patients) and is the most common reason for discontinuing treatment by patients [5, 6].
The human ocular surface requires vitamin A and its active derivatives, the retinoic acids, to maintain integrity. These retinoids regulate transcriptional levels of target genes through the activation of members of the retinoic acid receptor super-family [12]. Sufficient levels of vitamin A are essential for the development and maintenance of goblet cells in the conjunctiva, low levels of which is a risk factor for DED [13]. Topical vitamin A and other retinoids have been investigated for the treatment of DED [14,15,16,17]. The majority of clinical studies have demonstrated beneficial effects on a number of parameters including reversal of squamous metaplasia, increased tear production and increased goblet cells; however, to the best of our knowledge, none of these therapies have been approved or are currently in clinical development.
It has been suggested that the beneficial effects of retinoids on ocular health are mediated via retinoic acid receptor γ [18, 19]. An ophthalmic solution formulation of the selective retinoic acid receptor γ agonist palovarotene has undergone investigation for DED in a first-in-human phase I trial (NCT04762355; retrospectively registered). The purpose of this study was to evaluate the ocular and systemic safety, tolerability and pharmacokinetics (PK) of ascending doses of palovarotene ophthalmic solution (PVO-OS) in healthy adults.
2 Methods
2.1 Study Design
This was a single-centre, randomised, double-masked, vehicle-controlled study in healthy adults (NCT04762355; retrospectively registered). Active treatment was PVO-OS, at dose concentrations of 0.025, 0.05 and 0.10 mg/mL, administered once-daily (QD) or twice-daily (BID). The placebo control was vehicle-to-match PVO-OS consisting of 10 mM of phosphate buffer (pH 7.88 ± 0.02) and 1% polysorbate 80 in sterile water.
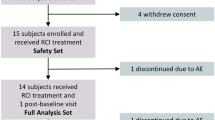
Participants were randomised at the time of treatment administration on day 1 in a 3:1 ratio to receive a one-dose regimen of either active treatment or vehicle (Fig. 1). A computerised randomisation scheme was created by a study centre statistician who was not involved with the data analysis. Individuals were assigned a four-digit randomisation number and a participant identification number.
Schematic of the study groups and study design. Participants were randomised at the time of treatment administration on day 1 in a 3:1 ratio to receive a one-dose regimen of either active treatment (palovarotene ophthalmic solution [PVO-OS]) or a vehicle. In total, 48 participants were randomised into the study: six to PVO-OS and two to the vehicle for each of the six groups. *Dosing and assessments for Groups 3 and 5 may have occurred simultaneously or sequentially with Groups 2 and 4, respectively. aBlood samples for the determination of PVO-OS systemic exposure were collected prior to once-daily (QD) dose administration, on days 8, 9 and prior to and following the QD dose on day 10 for Groups 1, 3 and 5. bBlood samples for the determination of PVO-OS systemic exposure were collected prior to AM twice-daily (BID) dose administration on days 5, 6 and prior to and following AM and PM BID dose administrations on day 7 for Groups 2, 4 and 6. PK pharmacokinetic
The active treatment in Groups 1, 3 and 5 was PVO-OS dosed QD at 0.025, 0.05 or 0.10 mg/mL, respectively. Both PVO-OS and the vehicle were administered by an eye drop in one eye on the first day of dosing (day 1). After a 2-day review period, participants received either PVO-OS or the vehicle QD in both eyes for 7 consecutive days.
The active treatment in Groups 2, 4 and 6 was PVO-OS dosed BID in both eyes at 0.025, 0.05 or 0.10 mg/mL, respectively. Participants in these active treatment groups and vehicle groups received study treatment in the morning (AM) and evening (PM; separated by 12 h) on the first day of dosing (day 1); this dosing continued for 7 consecutive days.
For Groups 1, 3 and 5, a review of data was conducted on day 3, to ensure that adequate safety and tolerability of PVO-OS had been demonstrated before the study could resume on day 4. Advancement of the study from the QD dosing regimen (Groups 1, 3 and 5) to the BID dosing regimen (Groups 2, 4 and 6), and escalation to the next dose regimen (Groups 3 and 5) also required safety review and approval.
The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation and Good Clinical Practice guidelines. The protocol, informed consent forms and other study documents were approved by an institutional review board, Advarra (Columbia, MD, USA).
2.2 Participants
Healthy male or female adults, 18–55 years of age, were eligible for this study. In addition, participants had to have a best-corrected visual acuity (BCVA) ≥70 as assessed by the Early Treatment Diabetic Retinopathy Study (ETDRS) letter score in both eyes. Individuals were not eligible for enrolment in the study if they had a history of any ocular or laser surgery within the 6 months prior to screening, or had a history or presence of any chronic eye disease other than refractive error, incipient cataract, strabismic amblyopia or anisometropic amblyopia. Participants were screened with a comprehensive ophthalmic examination (by an ophthalmologist) and received a physical examination and laboratory testing (by a family medicine physician). To further determine any underlying dry eye symptoms, individuals were asked a standardised list of questions at screening and for each study visit. A full list of inclusion and exclusion criteria is detailed in the Electronic Supplementary Material (ESM).
Participants were fully informed, agreed to participate in the study and signed an informed consent form.
2.3 Primary Endpoints
The primary objective was to assess the ocular and systemic safety and tolerability of single and multiple doses of PVO-OS at different concentrations in healthy adults. Safety was assessed by ocular and systemic assessments. The ocular endpoints included the number and severity of treatment-emergent ocular adverse events (TEOAEs) in the PVO-OS and vehicle treatment groups, and changes from baseline in ocular safety measurements as determined by BCVA, corneal fluorescein staining, tear break-up time, measurement of intraocular pressure (IOP), slit lamp examination, dilated fundal examination and assessment of ocular symptoms. All examinations were conducted by the same physician (William J. Foster) in a systematic manner, in the same order. The full schedule of assessments is available in Tables 1 and 2 of the ESM.
The systemic endpoint was the number and severity of treatment-emergent adverse events (TEAEs). Adverse events (AEs), including serious AEs, were collected from the time informed consent was granted until the end of study participation, which included a 14-day follow-up period for AE assessment. The investigator followed up on all AEs observed or reported by the participant up to the end of the reporting period or until the event had stabilised and follow-up was no longer necessary. AEs were classified by system organ class and preferred term using the Medical Dictionary for Regulatory Activities (version 21.0).
2.3.1 Ocular Safety Assessments: Best-Corrected Visual Acuity
Ocular assessments were performed on both eyes by an ophthalmologist, except for the BCVA, which was performed by trained site personnel under the supervision of an ophthalmologist. BCVA to assess ocular function was determined using a standard ETDRS chart at 4 m [20].
2.3.2 Corneal Fluorescein Staining
Fluorescein was used to stain the surface of the eye for evaluation of the epithelial surface of the cornea using a slit lamp microscope. Total corneal staining score was calculated by adding the individual grades from the central, superior, temporal, nasal and inferior regions of the corneal surface (Fig. 1 of the ESM). Staining for each region was graded 0–3 whereby: 0 (none) = no staining; 1 (mild) = 1–5 dots; 2 (moderate) = 6–15 dots; 3 (severe) = ≥ 16 dots, 1 or more areas of confluent staining, macro-staining (> 1 mm) or stained filaments [21].
2.3.3 Tear Break-Up Time
The tear break-up time described the stability of the tear film and was performed by observation through a slit lamp. Fluorescein was used to stain the surface of the eye and the upper eyelid was gently retracted. Tear break-up time was defined as the time it takes from the final blink until the first appearance of a dry spot, disruption of the tear film or the patient closed their eyes [21]. If the tear film remained stable for more than 60 s, the test was stopped at 60 s. Three consecutive recordings were taken in each eye.
2.3.4 Intraocular Pressure
IOP was measured in both eyes using a Goldmann applanation tonometer. Three separate IOP measurements per eye were performed and individual values were recorded.
2.3.5 Slit Lamp Examination
Slit lamp examination of the eyelids, conjunctiva, limbus, cornea, anterior chamber, iris, lens and anterior vitreous was performed without pupil dilation. Presence of eyelid erythema, eyelid swelling, Meibomian gland dysfunction, chemosis, conjunctival hyperaemia, corneal oedema, corneal opacity, ocular discharge, bulbar conjunctival injection, anterior chamber cells, anterior chamber flare and cataract was evaluated. Any other abnormality that was not noted above was also reported.
2.3.6 Dilated Fundus Examination
A dilated fundus examination was performed in both eyes. The pupils were dilated with Mydriacyl 1.0% and Mydfrin 2.5% (Alcon Laboratories, Inc., Fort Worth, TX, USA) after all other vision testing was completed. The vitreous, retina, macula, choroid and optic nerve were evaluated.
2.3.7 Other Safety Assessments
Safety was also determined by the evaluation of physical examinations, vital signs, electrocardiograms, clinical laboratory parameters and pregnancy tests for female individuals of childbearing potential.
2.4 Secondary Endpoints
The secondary objective of this study was to assess the systemic exposure of multiple doses of PVO-OS at different concentrations in healthy adults. Secondary endpoints included plasma concentrations of palovarotene after multiple ocular doses. The QD and BID dosing regimens were evaluated at doses of 0.75, 1.5 and 3.0 μg/eye (0.025, 0.05 and 0.10 mg/mL, respectively) given in both eyes for a total daily dose of 1.5, 3.0 and 6.0 μg for the QD regimen and 3.0, 6.0 and 12.0 μg for the BID regimen.
2.4.1 Pharmacokinetic Assessments and Statistical Analyses
This is a phase I study, not designed to measure effect size. Therefore, the sample size chosen for this study was not based on statistical considerations but was based on a protocol to introduce PVO-OS, never before studied in humans, safely. Blood samples for the determination of PVO-OS systemic exposure were collected: prior to QD dose administration on days 8 and 9 and prior to and following the QD dose on day 10 for Groups 1, 3 and 5; prior to AM BID dose administration on days 5 and 6 and prior to and following AM and PM BID dose administrations on day 7 for Groups 2, 4 and 6. Definitions of included PK parameters are provided in the ESM.
The main absorption and disposition parameters were estimated using a noncompartmental approach with a log-linear terminal phase assumption. The linear up/log down trapezoidal rule was used to estimate the area under the concentration–time curves (AUCs) and the terminal phase was estimated by maximising the coefficient of determination estimated from the log-linear regression model.
To assess the day at which steady state was considered to have been attained, the ln(log)-transformed pre-dose concentrations of days 8, 9 and 10 for Groups 1, 3 and 5 and on days 5, 6 and 7 for Groups 2, 4 and 6 were analysed by stratification of the group using Helmert contrasts, such that each timepoint was compared to the mean of the subsequent timepoint. Plasma concentrations were considered to have reached steady state when the day effect was not statistically significant at 5% for at least one of the comparisons.
3 Results
3.1 Participant Disposition and Baseline Demographics
Participants were screened and assessed sequentially, with screening for the subsequent cohort occurring after assessment of the previous cohort. Screening commenced in September 2018 with the last assessment visit in January 2019. A total of 141 individuals were screened, 74 of whom were deemed eligible for enrolment, the first 48 of which were randomised into the study: 36 to PVO-OS and 12 to vehicle. One participant treated with PVO-OS 0.10 mg/mL withdrew from the study on day 6 for reasons unrelated to clinical events and treatment was discontinued. Baseline demographics are described in Table 1 and were similar between those treated with PVO-OS and the vehicle.
3.2 Safety Evaluations
3.2.1 Treatment-Emergent Adverse Events
Overall, 116 and 23 TEAEs were reported by 29 (80.6%) and 8 (66.7%) participants treated with PVO-OS and the vehicle, respectively (Table 2). Additionally, 89 TEOAEs were reported by 22 individuals (61.1%) treated with PVO-OS and ten TEOAEs were reported by five (41.7%) of those treated with vehicle. The most commonly reported TEOAEs following PVO-OS administration were erythema, irritation and skin dryness of the eyelid, eye pruritus and eye irritation. A summary of the TEAEs reported by two or more participants is listed in Table 3. There were no deaths or serious AEs reported in the study.
Four participants (8.3%) discontinued because of TEAEs: two (5.6%) treated with PVO-OS 0.10 mg/mL (Group 6) experienced eyelid irritation and facial swelling (without throat, laryngeal or systemic symptoms); two (16.7%) who received the vehicle (one each in Groups 1 and 6) experienced elevated amylase and lip swelling, respectively. All TEAEs that led to discontinuation were mild or moderate, classed as possibly related to study treatment and resolved without sequelae.
3.2.2 Ocular Safety Assessments
At screening and baseline, the mean number of letters read for BCVA in each group ranged from 83.5 to 96.5. Over the course of the study, mean change (improvement or worsening) was fewer than five letters (e.g. one-line ETDRS). No participant lost 15 letters or more in any eye at any visit. The greatest loss was a transient loss of 11 letters in one eye in one participant in Group 2 on day 5, which was resolved at the final visit.
Five participants (13.9%) receiving PVO-OS (one in Group 1; three in Group 4; one in Group 6) and two in the vehicle-treated group (16.7%) had severe staining on a corneal fluorescein staining evaluation. Corneal fluorescein staining graded as severe was generally transient and limited to one quadrant. Slit lamp biomicroscopy demonstrated no abnormality of the cornea at the time of the finding and there were no associated visual acuity changes.
No meaningful decrease in tear break-up time was observed across the study groups. No TEOAEs related to increased IOP were observed. Transient increases in IOP of 10 mmHg and higher occurred in one participant treated with vehicle QD (Group 5) and in two participants after treatment with PVO-OS (one in Group 5 and one in Group 6). The single greatest increase in IOP was 13 mmHg experienced by one individual treated with the vehicle on day 3.
Overall, no clinically significant abnormalities were observed in ophthalmoscopy or dilated fundus examination assessments. No shifts from normal at baseline to abnormal at post-baseline visits in ophthalmoscopy examination were observed in this study.
Meibomian gland examination was generally normal, with infrequent instances of the vascularity of the eyelid margin and the plugging of the Meibomian gland being graded as mild. One participant treated with PVO-OS (Group 6) presented with Meibomian gland dysfunction in both eyes on day 8 and at the follow-up visit. The only AEs experienced by the individual were mild TEOAEs: erythema and irritation of the eyelid. These TEOAEs were experienced on day 6, approximately 1 h after dosing and were resolved at the end of the study.
Overall, 55.6% of participants treated with PVO-OS and 50.0% of those treated with the vehicle reported ocular symptoms following treatment. All were minimal or mild, with the exception of three individuals treated with PVO-OS reporting moderate-to-severe ocular symptoms. A summary of the moderate and severe ocular symptoms that occurred after treatment with PVO-OS are presented in Table 3 of the ESM.
No clinically significant individual vital sign abnormalities and no TEAEs related to vital sign assessments were reported. One participant treated with vehicle QD (Group 1) experienced a TEAE of an elevated amylase level on days 7 and 8; the amylase level returned to normal on day 11 and no other clinically significant laboratory changes were observed in this study. Clinically significant physical examination findings were found in six participants: one each in Group 1 (vehicle) and Group 2 (active treatment) and four in Group 4 (active treatment). All were ocular findings (generally associated with mild severity TEOAEs) except for one systemic finding of abdominal tenderness (Table 4 of the ESM). All TEAEs resolved within 4–15 days after occurrence.
3.3 Pharmacokinetic Analysis
Plasma palovarotene concentrations were generally measurable for up to 3–4 h for the 0.75 μg/eye and 1.5 μg/eye dose regimens and up to 12 h for the 3.0 μg/eye dose regimen independent of the frequency of administration (QD and BID) and the time of administration for BID (AM vs PM). Following QD and BID dosing regimens, palovarotene rapidly appeared in plasma with a median time to reach the maximum observed concentration that ranged from 0.5 to 1.0 h after drug administration across the dose range tested (Fig. 2a).
Plasma concentration–time profiles of palovarotene ophthalmic solution (PVO-OS). a Mean palovarotene plasma concentration–time profiles (linear scale) following once-daily (QD) and twice-daily (BID) administration of PVO-OS. b Box plots of mean maximum observed concentration (Cmax) following QD and BID administration of PVO-OS. c Box plots of the area under the concentration–time curve (AUCtau) following QD and BID administration of PVO-OS. Each box contains the 25th and the 75th percentiles, arithmetic mean (solid line) and median (dashed line). Error bars are standard deviation
Following QD administration of palovarotene, the mean maximum observed concentration at steady state ranged from 12.4 pg/mL (0.75 μg/eye) to 58.2 pg/mL (3.0 μg/eye), increasing approximately five-fold for a four-fold increase in dose (Fig. 2b). The mean AUCtau ranged from 23.7 h∙pg/mL (0.75 μg/eye) to 245 h∙pg/mL (3.0 μg/eye), increasing approximately ten-fold for a four-fold increase in dose (Fig. 2c).
Palovarotene PK parameters are summarised in Table 5 of the ESM for the QD treatment groups and in Table 6 of the ESM for the BID treatment groups. Overall, the maximal exposure observed at the highest dose of 3.0 μg/eye (0.10 mg/mL) BID (AUC0–24 h) was 436 h∙pg/mL. Following BID administration of PVO-OS, the PK profile of the AM dose was similar to the PM dose.
4 Discussion
Current therapies specifically approved for DED management mediate symptom relief through anti-inflammatory pathways [6, 22]. However, as highlighted at the Tear Film and Ocular Surface Society Dry Eye Workshop II, better tolerated and more efficient therapies are needed using different modes of formulation and/or new anti-inflammatory or immunomodulating agents [23, 24]. Furthermore, while inflammation is an appropriate therapeutic target for many patients with DED, there is a need for therapies that address the underlying issues in DED beyond inflammation [25]. Given that DED develops because of a vicious cycle of tear film instability, tear hyperosmolarity, apoptosis, inflammation and a loss of mucin-producing goblet cells; if the underlaying cause of inflammation is not addressed, more damage to the tear film can occur [26]. Such disease-modifying therapies would offer the potential to obtain an enduring clinical benefit, and could potentially improve the QoL of many patients. Dry eye disease can substantially degrade QoL through pain and irritation, affect ocular and general health, well-being and perception of visual function as well as impact visual performance. In its more severe forms, DED can be debilitating and result in both psychological and physical effects that impact QoL [2]. Therefore, an unmet need exists for therapeutic options that may address the underlying causes of DED, leading to improvement of both eye and general public health [2, 25].
Here, the ocular and systemic safety, tolerability and pharmacokinetics of single and multiple doses of PVO-OS were assessed in healthy adults enrolled in a phase I trial. The administration of PVO-OS was generally well tolerated at doses up to 0.10 mg/mL administered BID, and no serious AEs were reported. These safety findings were consistent across biomicroscopy, ophthalmoscopy and AEs. With higher concentrations and frequencies of PVO-OS dosing, the occurrence of erythema, irritation and skin dryness of the eyelid, as well as pruritus, were reported. These events were mild and transient and no participant lost 15 letters (three lines ETDRS) of vision, indicating that PVO-OS did not adversely affect visual acuity during the study period [20].
In this study, the overall incidence of ocular AEs in participants treated with PVO-OS increased with ascending dose and frequency compared with those treated with vehicle, suggesting that lower concentrations of PVO-OS may be most appropriate. However, there were no significant changes in vital signs and electrocardiogram parameters at any dose regimens, and there were no significant trends observed in changes of laboratory parameters.
Similar PK profiles were observed for the QD and BID regimens following multiple ascending doses of PVO-OS; following QD dosing, the maximum palovarotene plasma concentration increased five-fold for a four-fold increase in dose. No meaningful difference was observed between the PK profile of PVO-OS following the AM and PM doses of the BID treatment. Overall, PVO-OS demonstrated favourable systemic safety; the maximal exposure observed at the highest dose of 3.0 μg/eye (0.10 mg/mL) BID (AUC0–24 h 436 h·pg/mL) was approximately 100-fold less than that observed following an oral 1 mg daily dose of palovarotene in healthy participants (AUC0–T ~46 h·ng/mL; unpublished data). Future studies might assess the intraocular concentration and PVO-OS kinetics.
No clinical studies to date have been conducted with PVO-OS. However, clinical studies have been conducted with oral palovarotene; with the exception of an increased risk of premature physeal closure identified in skeletally immature children with fibrodysplasia ossificans progressiva, the risks associated with oral administration of palovarotene are generally consistent with those observed with marketed non-selective retinoids in other indications [27]. AEs that may be experienced include, but are not limited to: mucocutaneous reactions, ocular complications and musculoskeletal and central nervous system effects [27, 28]. Given the established safety profile of oral systemic retinoids and potential concerns, the safety and PK data from this study suggest that the administration of PVO-OS was generally well tolerated and there were fewer systemic safety concerns than with oral retinoids. However, these assessments necessitated a smaller sample size and were conducted in healthy individuals. The sample size chosen for this study was not based on statistical considerations. Power calculations are most appropriate for studies for which the primary focus is null hypothesis significance testing and statistical estimation (concerned, for example with sampling distributions, and interval estimation). In this phase I study, the goal was not to make inferences, compare groups or assess the probability that study results are true. Rather, the primary endpoint was to assess the ocular and systemic safety and tolerability of single and multiple doses of a new formulation of a compound never before tested in humans [29].
Further, although very limited data exist on the potential effect of race or ethnicity on dry eye prevalence, data from the Women’s Health Study suggest that the prevalence of severe symptoms and/or clinical diagnosis of DED may be greater in Hispanic or Asian women, as compared with Caucasian women [30]. Therefore, the generalisability of these results to all patients with DED is limited, and further evaluation in a phase II/III study is required to assess the therapeutic potential of PVO-OS for the treatment of DED.
5 Conclusions
The administration of PVO-OS was generally well tolerated at doses up to and including 0.10 mg/mL BID and was primarily associated with the occurrence of erythema, irritation and skin dryness of the eyelid. Similar PK profiles were observed for the QD and BID regimens following multiple ascending doses of PVO-OS. These data support further investigation of the safety and efficacy profile of PVO-OS in patients with DED.
References
Nelson JD, Craig JP, Akpek EK, Azar DT, Belmonte C, Bron AJ, et al. TFOS DEWS II Introduction Ocul Surf. 2017;15:269–75.
The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:93–107. https://pubmed.ncbi.nlm.nih.gov/17508117/.
Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112:71–82.
Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:163–78. https://pubmed.ncbi.nlm.nih.gov/17508120/.
Javadi M-A, Feizi S. Dry eye syndrome. J Ophthalmic Vis Res. 2011;6:192–8.
O’Neil EC, Henderson M, Massaro-Giordano M, Bunya VY. Advances in dry eye disease treatment. Curr Opin Ophthalmol. 2019;30:166–78.
Novack GD. Repurposing medications. Ocul Surf. 2020;19:336–40.
Haber SL, Benson V, Buckway CJ, Gonzales JM, Romanet D, Scholes B. Lifitegrast: a novel drug for patients with dry eye disease. Ther Adv Ophthalmol. 2019;11:2515841419870366.
Baudouin C, Irkeç M, Messmer EM, Benítez-del-Castillo JM, Bonini S, Figueiredo FC, ODISSEY European Consensus Group Members, et al. Clinical impact of inflammation in dry eye disease: proceedings of the ODISSEY group meeting. Acta Ophthalmol. 2018;96:111–9.
Taylor M, Ousler G, Torkildsen G, Walshe C, Fyfe MCT, Rowley A, et al. A phase 2 randomized, double-masked, placebo-controlled study of novel nonsystemic kinase inhibitor TOP1630 for the treatment of dry eye disease. Clin Ophthalmol. 2019;13:261–75.
White DE, Zhao Y, Jayapalan H, Machiraju P, Periyasamy R, Ogundele A. Treatment satisfaction among patients using anti-inflammatory topical medications for dry eye disease. Clin Ophthalmol. 2020;14:875–83.
Nezzar H, Chiambaretta F, Marceau G, Blanchon L, Faye B, Dechelotte P, Rigal D, Sapin V. Molecular and metabolic retinoid pathways in the human ocular surface. Mol Vis. 2007;13:1641–50.
Milner MS, Beckman KA, Luchs JI, Allen QB, Awdeh RM, Berdahl J, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders: new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;27(Suppl. 1):3–47.
Kim EC, Choi JS, Joo CK. A comparison of vitamin a and cyclosporine a 0.05% eye drops for treatment of dry eye syndrome. Am J Ophthalmol. 2009;147:206-13.e203.
Kobayashi TK, Tsubota K, Takamura E, Sawa M, Ohashi Y, Usui M. Effect of retinol palmitate as a treatment for dry eye: a cytological evaluation. Ophthalmologica. 1997;211:358–61.
Selek H, Unlü N, Orhan M, Irkeç M. Evaluation of retinoic acid ophthalmic emulsion in dry eye. Eur J Ophthalmol. 2000;10:121–7.
Tseng SC, Maumenee AE, Stark WJ, Maumenee IH, Jensen AD, Green WR, et al. Topical retinoid treatment for various dry-eye disorders. Ophthalmology. 1985;92:717–27.
Kimura K, Orita T, Liu Y, Yang Y, Tokuda K, Kurakazu T, et al. Attenuation of EMT in RPE cells and subretinal fibrosis by an RAR-γ agonist. J Mol Med. 2015;93:749–58.
Liu Y, Kimura K, Orita T, Suzuki K, Teranishi S, Mori T, Sonoda K-H. Inhibition by a retinoic acid receptor γ agonist of extracellular matrix remodeling mediated by human Tenon fibroblasts. Curr Opin Ophthalmol. 2015;21:1368–77.
Beck RW, Maguire MG, Bressler NM, Glassman AR, Lindblad AS, Ferris FL. Visual acuity as an outcome measure in clinical trials of retinal diseases. Ophthalmology. 2007;114:1804–9.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
White DE, Zhao Y, Ogundele A, Fulcher N, Acs A, Moore-Schiltz L, et al. Real-world treatment patterns of cyclosporine ophthalmic emulsion and Lifitegrast ophthalmic solution among patients with dry eye. Clin Ophthalmol. 2019;13:2285–92.
Craig JP, Nelson JD, Azar DT, Belmonte C, Bron AJ, Chauhan SK, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15:802–12.
Cursiefen C, Cordeiro F, Cunha-Vaz J, Wheeler-Schilling T, Scholl HPN. Unmet needs in ophthalmology: a European Vision Institute-Consensus Roadmap 2019–2025. Ophthalmic Res. 2019;62:123–33.
Dunn JD, Karpecki PM, Meske ME, Reissman D. Evolving knowledge of the unmet needs in dry eye disease. Am J Manag Care. 2021;27:S23-32.
Baudouin C, Messmer EM, Aragona P, Geerling G, Akova YA, Benítez-del-Castillo J, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100:300–6.
Mills CM, Marks R. Adverse reactions to oral retinoids. Drug Saf. 1993;9:280–90.
Desai A, Kartono F, Del Rosso JQ. Systemic retinoid therapy: a status report on optimal use and safety of long-term therapy. Dermatol Clin. 2007;25:185–93.
Bell ML, Whitehead AL, Julious SA. Guidance for using pilot studies to inform the design of intervention trials with continuous outcomes. Clin Epidemiol. 2018;10:153–7.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26.
Acknowledgements
The authors thank all participants involved in the study, as well as investigators and research staff in the participating institution. The authors thank Marc Lynch, PhD and Amelia Frizell-Armitage, PhD, of Costello Medical, Cambridge, UK for providing medical writing support, which was sponsored by Ipsen in accordance with Good Publication Practice guidelines.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Ipsen.
Conflicts of Interest/Competing Interests
WJF is a consultant for Altasciences. ALS is an employee of Ipsen. KWS has no financial disclosures. JMR was an employee of Ipsen at the time the study was conducted.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Qualified researchers may request access to patient-level study data that underlie the results reported in this publication. Additional relevant study documents, including the clinical study report, study protocol with any amendments, annotated case report form, statistical analysis plan and dataset specifications may also be made available. Patient-level data will be anonymised and study documents will be redacted to protect the privacy of study participants. Where applicable, data from eligible studies are available 6 months after the studied medicine and indication have been approved in the USA and European Union or after the primary manuscript describing the results has been accepted for publication, whichever is later. Further details on Ipsen’s sharing criteria, eligible studies and process for sharing are available here (https://vivli.org/members/ourmembers/). Any requests should be submitted to www.vivli.org for assessment by an independent scientific review board.
Code Availability
Not applicable.
Authors’ Contributions
Substantial contributions to study conception and design: WJF, ALS, JMR; substantial contributions to analysis and interpretation of the data: WJF, ALS, KWS, JMR; drafting the article or revising it critically for important intellectual content: WJF, ALS, KWS, JMR; final approval of the version of the article to be published: WJF, ALS, KWS, JMR.
Data Sharing
Not applicable.
Additional information
James M. Roach: was an employee of Ipsen at the time the study was conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Foster, W.J., Strahs, A.L., Small, K.W. et al. A Randomised Phase I Study to Assess the Safety, Tolerability and Pharmacokinetics of Palovarotene Ophthalmic Solution. Drugs R D 23, 43–53 (2023). https://doi.org/10.1007/s40268-022-00410-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-022-00410-6