Abstract
Objectives
The COVID-19 pandemic resulted in a particularly adverse and stressful environment for expecting mothers, possibly enhancing feelings of anxiety and parenting stress. The present work assesses mothers' anxiety levels at delivery and parenting stress after 3 months as moderated by home-visiting sessions.
Methods
Women (n = 177) in their second or third trimester of pregnancy during the COVID-19 lockdown were enrolled in northern Italy and split into those who did and did not receive home visits. After 3 months, the association between anxiety at delivery and parenting stress was assessed with bivariate correlations in the whole sample and comparing the two groups.
Results
Higher anxiety at birth correlated with greater perceived stress after 3 months. Mothers who received at least one home-visiting session reported lower parenting stress at 3 months than counterparts who did not receive home visits.
Conclusions for Practice
The perinatal period is a sensitive time window for mother-infant health, especially during a critical time like the COVID-19 pandemic. We suggest that home-visiting programs could be beneficial during global healthcare emergencies to promote maternal well-being after delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on this topic Adverse conditions, such as the pandemic, during developmental windows of heightened plasticity increase the risk of maladaptive stress responses. Both pregnancy and the postnatal period represent a time of exceptional environmental sensitivity for mothers and infants. Home-visiting programs may be beneficial in increasing mothers’ self-confidence, protecting them from developing severe affective symptoms and parenting stress.
What this study adds Home-visiting reduces parental stress, protecting the dyadic interactive aspects of the mother-infant relationship. Home visits are specifically beneficial for mothers who present high anxiety levels after delivery and provide a social resource, contrasting the isolation and trauma experienced during the COVID-19 pandemic. These results have both research and clinical implications and may inform healthcare policies for mother-infant health.
Introduction
The COVID-19 pandemic is an unprecedented global healthcare emergency and a collective traumatic experience (Bo et al., 2021; Kanzler & Ogbeide, 2020). The high rates of SARS-CoV-2 contagion, its rapid spread, the partial availability of effective treatments or vaccines, together with social distancing and economic challenges implied by mitigation and containment strategies, contribute to relevant distress and raise concerns for public health (Graffigna et al., 2021; Ozamiz-Etxebarria et al., 2020). Previous literature has extensively demonstrated that individuals exposed to such intense adverse conditions during developmental windows of heightened plasticity (Kim, 2016) may be susceptible to developing maladaptive stress responses and affective symptoms (Davis & Narayan, 2020; Pluess & Belsky, 2011). Consistently, it is of paramount importance to study the impact of pandemic-related stress on the health of individuals who are experiencing sensitive periods and the protective role of preventive and supportive interventions (Horesh & Brown, 2020; Provenzi & Tronick, 2020).
Both pregnancy and the postnatal (i.e., the first 3 months after birth) period represent an exceptionally sensitive time for mothers and infants. Not surprisingly, reports of affective symptoms are not uncommon in the post-partum. During the pre-pandemic period (i.e., before March 2020, when lockdown began in Italy due to the outbreak of the coronavirus disease), the prevalence of full-blown depressive symptomatology was estimated in 10–15% of women after delivery in a meta-analysis of 291 studies from 56 countries (Hahn-Holbrook et al., 2018); whereas clinically relevant anxiety symptoms were observed in 10% of mothers in a meta-analysis of 102 studies from 34 countries (Dennis et al., 2017). Meta-analytic evidence suggested that levels of post-natal depression in mothers have increased during the present pandemic (Hessami et al., 2020). Nonetheless, anxiety is the most reported psychological symptom in pregnant women and new mothers in different countries hit by the COVID-19 healthcare emergency (Cameron et al., 2020; Racine et al., 2021; Salehi et al., 2020). Notably, in a recent report from our group on a cohort of 281 mothers, the rates of clinically relevant symptoms of depression and anxiety during the pandemic were 26 and 32%, respectively (Grumi et al., 2021).
Another well-documented consequence of maternal reduced mental health in the post-partum period is an increase in parenting stress (Larkin & Otis, 2019). This pattern has been defined as the maternal difficulty in adapting to the parental role, possibly due to an overload of perceived requests arising from the demands of the parental role and the sense of not having the resources to absolve them, resulting in psychological distress and depressive states (Gray et al., 2012; Phetrasuwan & Shandor Miles, 2009). Parenting stress is multi-dimensional and only partly depends on maternal psychological adjustment to the transition to motherhood; rather, it includes two relevant dimensions related to caregiving burden and the presence of infants’ difficult, temperamental traits. The different subdimensions of parenting stress largely contribute to the quality of the post-natal caregiving environment, and they may contribute to the association between maternal mental health and infants' developmental outcomes. For instance, Sheinkopf et al. (2006) have reported that the link between neonatal characteristics and temperament might be moderated by maternal parenting stress in a large cohort of at-risk infants exposed to prenatal stress. Among the dimensions of parenting stress, the presence of a dysfunctional or problematic interactive pattern between mother and infant, such as lack of responsiveness, passivity or intrusiveness, low expression of positive affect, withdrawal or avoidance, is of critical concern (Reck et al., 2004; Sheinkopf et al., 2006). As for the COVID-19 emergency, a Chinese study has shown that levels of maternal parenting stress dramatically increased from before to during the pandemic (Tchimtchoua Tamo, 2020). Additionally, post-natal maternal parenting stress has been a significant variable involved in the association between maternal pandemic-related anxiety and later infant temperament at 3 months in Italian mothers (Provenzi et al., 2021).
Home-visiting programs may be beneficial, as they provide a supportive intervention that can increase mothers’ sense of self-confidence and competence as a parent, thus protecting them from developing severe affective symptoms and parenting stress during the first months after delivery (Liu et al., 2012). Despite the existence of different methodological approaches to home-visiting, previous research documented positive effects on maternal health and child development for all of them. For example, a recent study found that a home-visiting program involving first-time mothers at risk, from three to 12 months after their child’s birth, reduced depression, anxiety, and parenting stress (Vismara et al., 2020). Moreover, a review of 21 relevant studies outlined significant improvements to the development and health of young children as a result of home-visiting (Peacock et al., 2013). In particular, the visits prevented child abuse in some cases, and in other instances, developmental benefits concerning cognition, behavioral problems, and, less consistently, language skills. Notably, previous research has mainly focused on the effects of home visits in mothers with moderate or severe depressive symptoms. The study of home-visiting effects in mothers with clinical risk for anxiety disorder is less documented. At the same time, such programs may be especially needed during a healthcare emergency such as the COVID-19, characterized by reduced social support and increased health-related worries in pregnant women (Williams et al., 2021).
In the present study, we report on an Italian cohort of mothers who were in the second or third trimester of pregnancy during the initial outbreak of the COVID-19 pandemic in Italy. The enrolled mothers retrospectively rated the severity of their anxiety symptoms at delivery, reported if they had received at least one home-visiting session from birth to 3 months of their infant’s age, and provided a quantitative estimate of parenting stress at their infant 3-month-age. The main goal was to assess significant differences in the parenting stress levels reported by mothers who received and those who did not receive home-visiting interventions during the pandemic. We hypothesized that mothers who received home visits would disclose less parenting stress than counterparts who did not participate in home-visiting programs. Moreover, we further explored this association controlling for the presence of clinically relevant anxiety levels at delivery. In the absence of previous data, no direction was hypothesized for the findings, and this second aim was exploratory.
Methods
Participants
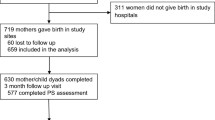
This study is part of the longitudinal and multi-centric Measuring the Outcomes of Maternal COVID-19-related Prenatal Exposure (MOM-COPE) research project (Provenzi et al., 2020). Eligible subjects were women in their second or third trimester of pregnancy during the months of the COVID-19 outbreak in northern Italy. No screening on postpartum mood disorder risk was performed. Rather, the opportunity of home-visits was handed to all women at the end of the antenatal classes. They were enrolled between May and October 2020 from ten neonatal units of territorial hospitals located in large provinces of northern Italy (e.g., Pavia, Piacenza, Lodi, Brescia, Cremona, Milano). At the time of the present analyses, 263 women were contacted, and 216 (82.1%) women accepted to participate in the study. Mothers were included if at least 18-year-old, in the absence of prenatal and postnatal diseases or injuries, if they delivered at term (i.e., from 37 + 0 to 41 + 6 gestational age), and if they tested negative for COVID-19 at delivery. Mothers were first contacted at antepartum classes or immediately following the post-partum period. The attrition rate between delivery and 3-month data collection time points was 18.1%, as 39 mothers did not provide complete data for the present analyses. Consistently, a sample of 177 women was available for the present study. The study was approved by the Ethics Committee of Pavia (protocol ID: 20200037366; ClinicalTrials.gov Identifier: NCT04540029) and the participating hospitals. All mothers provided informed consent to participate in the study.
Procedure
Socio-demographic (i.e., maternal age, educational level, and occupational status) and neonatal data (i.e., sex, mode of delivery, gestational age, birth weight, head circumference, length, Apgar score at 5 min) were obtained from medical records. Within 48 h from delivery, the mothers filled in a self-report questionnaire rating their anxiety symptoms, namely the state subscale of the State-Trait Anxiety Inventory (STAI-Y) (Pedrabissi & Santinello, 1989; Spielberger, 1989). The theoretical range for the STAI-Y continuous raw score is between 20 and 80, and a score of 40 is a reliable cut-off for clinically relevant anxiety risk (Julian, 2011). The Cronbach’s Alpha was .94. At the 3-month age of their infants, mothers further reported on their concurrent parenting stress by filling in the Parenting Stress Index Short Form, PSI-SF (Abidin, 1983; Guarino et al., 2008). This questionnaire includes 36 items that provide a global score of parental stress and three subscales' scores: (1) Parental Distress (PD): evaluates distress experienced in the parental role, directly related to the demand of the role or resulting from personal factors (e.g., conflicts with the partner, depression, lack of social support); (2) Difficult Child (DC): assesses whether parents perceive controlling their children in terms of their behavioral traits as easy or difficult (measuring the child’s self-regulatory abilities as perceived by the parent); (3) Parent–Child Dysfunctional Interactions (PCDI): indexes parents’ perception of whether their child meets their expectations or not, and how satisfied they are in the relationship with their own child; (4) Total Stress scale: obtained from the sum of the three subscales. It indicates the overall degree of stress that parents experience in their role as parents. The Cronbach’s Alpha was .95. Moreover, mothers retrospectively reported on whether they received home-visiting sessions after delivery further detailing the number of sessions and their satisfaction for the program, including ratings for (a) satisfaction for themes addressed during the sessions, (b) satisfaction for the relationship with the home-visitor, (c) appropriateness of sessions with respect to their expectations.
Analytical Plan
Mothers who received at least one home-visiting session were compared to counterparts who did not receive home-visiting for the total and subscale scores of the PSI-SF by means of independent-sample t-tests. The chi-squared test was used to compare the distribution of clinically relevant anxiety symptoms between the two groups. The association between anxiety levels at delivery (identified by the STAI-Y questionnaire) and parenting stress in the whole group was assessed by means of bivariate correlation; the same analysis was repeated separately for mothers who received and those who did not receive home-visiting sessions. All analyses were conducted using IBM SPSS 27 for Windows, setting p < 0.05.
Results
Participants’ descriptive statistics are reported in Table 1.
Fifty-four (31%) mothers received at least one home-visiting session. Of these mothers, thirty-nine received only one session (72%), nine received two sessions (17%), and six received three or more visits (11%). In the whole sample, forty-eight mothers (27%) reported anxiety levels above the clinical risk cut-off. The percentage of clinically relevant anxiety symptoms did not show a statistically significant difference between mothers who received home-visiting (n = 13, 24%) and those who did not (n = 35, 28%), χ2(1) = .364, p = .546. The maternal subjective ratings of appreciation for the single aspects of home-visiting sessions are reported in Table 2.
The overall satisfaction was high for both general expectations (with a mean rating of 4.8 out of 6, SD = 0.08) and the relationship with the operator (mean rating of 5.4 out of 6, SD = 0.31).
Anxiety levels at birth measured through the STAI-Y did not differ between the two groups of mothers (all ps > 0.05). 3 months after delivery, mothers who received at least one home-visiting session reported lower stress in the PCDI subscale of the PSI-SF compared to counterparts who did not receive home-visiting, t (175) = 2.11, p = .037 (Fig. 1).
Parenting stress scores in mothers who received at least one home-visiting session and in counterparts who did not receive any home-visiting session. For each boxplot, red dots represent mean values, the horizontal line represents the median value, whiskers indicate min and max values, and box segments the distribution between first and third quartiles (Color figure online)
No statistically significant differences emerged for the other PSI-SF subdomains and Total Stress score between mothers who received and those who did not receive home-visiting sessions. The correlation between the continuous scores of maternal anxiety and each of the parenting stress subdomains was then analyzed, and the scores are reported in the matrix in Fig. 2.
In the whole sample, significant associations emerged between maternal anxious symptoms after delivery and 3-month parenting stress for all subscales of the PSI-SF (all ps < .05). In general, higher anxiety levels at delivery corresponded to higher parenting stress reported after 3 months. Notably, when the correlation between anxiety levels at delivery and parenting stress was assessed separately for mothers who received and those who did not receive home-visiting sessions, the correlation between anxiety and PCDI was significant, r = .36, p < .001, in the group of mothers who did not receive home-visiting whereas it was not for mothers who received at least one session, r = .058, p = .676 (Fig. 3).
Discussion
This study aimed to identify the possible beneficial effects of home-visiting programs in reducing parenting stress in mothers and reducing the risk of increased parenting stress in mothers who showed high levels of anxiety after delivery during an unprecedented global traumatic experience such as the COVID-19 pandemic.
Our results showed that home-visiting was associated with lower parental stress in the subscale of Parent–Child Dysfunctional Interactions (PCDI), while no decrease in stress scores was observed for the other subdomains. Therefore, the beneficial effects of post-natal home visits were observed for a specific component of parenting stress that reflects the dyadic interactive aspects of the mother-infant relationship. In contrast, the other two subdomains (i.e., Parental Distress and Difficult Child) provide quantitative estimates of maternal stress related to individual sources. This finding can be better understood considering that the primary goal of home-visiting sessions is not to reduce individual maternal distress or to provide behavioral interventions for child behavior regulation. Rather, home visits are directed explicitly at increasing maternal feelings of self-confidence, competence as a parent, and perception of social support (Liu et al., 2012). As such, the fact that this early preventive support might be effective in reducing the risk of stress arising from potential issues in parent-infant interaction is not surprising and extend previous evidence on the benefit of home visiting programs (Castel et al., 2016; Kaaresen et al., 2006; Kiani et al., 2021) to the current pandemic time. Indeed, it should be highlighted that in rating their satisfaction towards the intervention, all mothers reported that they felt helped in breastfeeding, understanding their child's behavior, obtaining information about physical and emotional development, and feeling more competent as a parent. Interestingly, even higher rates were given to those aspects that involved the relationship with the care provider, such as feeling heard, supported, having the opportunity of asking questions and expressing doubts. Mothers felt that they were less alone, not judged and that they had someone they could trust (Table 2). Mirroring the findings that showed how the dyadic interactive aspects of mother-infant relationship were the ones that benefitted more from the intervention, we confirm that the social connections and support are the core of a heightened well-being perception in mothers who were exposed to social separations during pregnancy. Home-visiting may provide a social resource in the face of the isolation and trauma experienced by expecting mothers during the COVID-19 pandemic (Provenzi & Tronick, 2020).
It should be highlighted that parenting stress was found to be significantly correlated with maternal anxiety in this cohort. Nonetheless, the statistical significance was confirmed only for the latter when controlling for this association in the home-visiting and non-home-visiting groups. As the two groups did not differ in the prevalence of clinically significant anxiety, this finding further supports the hypothesis that home visiting programs should be specifically beneficial for mothers who present high levels of anxiety after delivery. In other words, home-visiting appears to be a source of protection for maternal mental health and the development of a nurturing caregiving environment, particularly during a global healthcare emergency. As delivering home-visiting programs to mothers during the first 3 months may act as a buffer between maternal anxiety and parenting stress, these preventive interventions are largely warranted to be offered to mothers regularly (Kersten-Alvarez et al., 2010; Rotheram-Borus et al., 2014).
A limit of the present study is that most mothers received only one home-visiting intervention (in the 72% of cases). The home-visiting programs are generally more beneficial with the increase in the number of visits (Nygren et al., 2018). The lower time dedicated to building parenting skills and confidence might be responsible for the lack of a general decrease in stress perceived by the mothers in our sample. Moreover, we reported an Italian cohort of mothers only. Thus, the generalization of our results might not always be possible, as different cultures and social structures greatly influence perceived support and stress (Campos & Kim, 2017). Keeping the focus on providing information about the child’s physical health and child development, other than supporting the parent–child relationship, is critically important. Finally, the satisfaction about the home-visiting program was reported retrospectively, and parenting stress was measured through a self-report scale. Having direct measures of such aspects might increase sensitivity in detecting changes in stress and allow a more controlled analysis of what home visits contribute to these changes.
Conclusions
In conclusion, the challenges of facing a pandemic imply a significant amount of additional stress, especially in such crucial phases as pregnancy, delivery, and the first post-natal months. Importantly, for those cases where, due to an individual predisposition or especially detrimental conditions, anxiety is predominant, a heightened risk of parental stress is indeed present. This is precisely where a home-visiting program can be fundamental towards effectively reducing the risks for both mothers and infants. Future clinical implications might consider using home-visit programs as an essential tool to improve parent–child interactions during a pandemic. Indeed, the COVID-19 emergency requires us to bridge the existing gap between research and clinical practice implementing, amongst several aspects, smart diagnostics, effective prevention, and compassionate communication (Horesh & Brown, 2020). We believe that screening anxiety levels in mothers after delivery might help detect those cases of heightened risk where implementing house-visiting programs that limit COVID-19- specific trauma in the first year of infants’ life would be of foremost importance.
Data Availability
The data included in this study have been made available on a permanent third-party archive (Zenodo) at this link: https://doi.org/10.5281/zenodo.7104124; further requests can be sent via email to the corresponding author.
Code Availability
No custom code was used.
References
Abidin, R. R. (1983). Parenting Stress Index: Manual, administration booklet,[and] Research Update.
Bo, H.-X., Li, W., Yang, Y., Wang, Y., Zhang, Q., Cheung, T., Wu, X., & Xiang, Y.-T. (2021). Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological Medicine, 51(6), 1052–1053. https://doi.org/10.1017/S0033291720000999
Cameron, E. E., Joyce, K. M., Delaquis, C. P., Reynolds, K., Protudjer, J. L. P., & Roos, L. E. (2020). Maternal psychological distress & mental health service use during the COVID-19 pandemic. Journal of Affective Disorders, 276, 765–774. https://doi.org/10.1016/j.jad.2020.07.081
Campos, B., & Kim, H. S. (2017). Incorporating the cultural diversity of family and close relationships into the study of health. American Psychologist, 72(6), 543–554. https://doi.org/10.1037/amp0000122
Castel, S., Creveuil, C., Beunard, A., Blaizot, X., Proia, N., & Guillois, B. (2016). Effects of an intervention program on maternal and paternal parenting stress after preterm birth: A randomized trial. Early Human Development, 103, 17–25. https://doi.org/10.1016/j.earlhumdev.2016.05.007
Davis, E. P., & Narayan, A. J. (2020). Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Development and Psychopathology, 32(5), 1625–1639. https://doi.org/10.1017/S0954579420001121
Dennis, C.-L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and post-natal anxiety: Systematic review and meta-analysis. British Journal of Psychiatry, 210(5), 315–323. https://doi.org/10.1192/bjp.bp.116.187179
Graffigna, G., Palamenghi, L., Savarese, M., Castellini, G., & Barello, S. (2021). Effects of the COVID-19 emergency and national lockdown on Italian citizens’ economic concerns, government trust, and health engagement: Evidence from a Two-wave Panel Study. The Milbank Quarterly, 99(2), 369–392. https://doi.org/10.1111/1468-0009.12506
Gray, P. H., Edwards, D. M., O’Callaghan, M. J., & Cuskelly, M. (2012). Parenting stress in mothers of preterm infants during early infancy. Early Human Development, 88(1), 45–49. https://doi.org/10.1016/j.earlhumdev.2011.06.014
Grumi, S., Provenzi, L., Accorsi, P., Biasucci, G., Cavallini, A., Decembrino, L., Falcone, R., Fazzi, E. M., Gardella, B., Giacchero, R., Guerini, P., Grossi, E., Magnani, M. L., Mariani, E. M., Nacinovich, R., Pantaleo, D., Pisoni, C., Prefumo, F., Sabatini, C., Scelsa, B., Maria V. S., Arsenio, S., Roberto, G., Simona, O., & Borgatti, R. (2021). Depression and anxiety in mothers who were pregnant during the COVID-19 outbreak in Northern Italy: The role of pandemic-related emotional stress and perceived social support. Frontiers in Psychiatry, 12, 716488. https://doi.org/10.3389/fpsyt.2021.716488
Guarino, A., Di Blasio, P., D’Alessio, M., Camisasca, E., & Serantoni, M. (2008). Parenting stress index short form: Adattamento italiano. Firenze: Giunti, Organizzazioni Speciali.
Hahn-Holbrook, J., Cornwell-Hinrichs, T., & Anaya, I. (2018). Economic and health predictors of national postpartum depression prevalence: A systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Frontiers in Psychiatry, 8, 248. https://doi.org/10.3389/fpsyt.2017.00248
Hessami, K., Romanelli, C., Chiurazzi, M., & Cozzolino, M. (2020). COVID-19 pandemic and maternal mental health: A systematic review and meta-analysis. The Journal of Maternal-Fetal & Neonatal Medicine. https://doi.org/10.1080/14767058.2020.1843155
Horesh, D., & Brown, A. D. (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 331–335. https://doi.org/10.1037/tra0000592
Julian, L. J. (2011). Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care & Research, 63(S11), S467–S472. https://doi.org/10.1002/acr.20561
Kaaresen, P. I., Ronning, J. A., Ulvund, S. E., & Dahl, L. B. (2006). A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics, 118(1), e9–e19. https://doi.org/10.1542/peds.2005-1491
Kanzler, K. E., & Ogbeide, S. (2020). Addressing trauma and stress in the COVID-19 pandemic: Challenges and the promise of integrated primary care. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S177–S179. https://doi.org/10.1037/tra0000761
Kersten-Alvarez, L. E., Hosman, C. M. H., Riksen-Walraven, J. M., Van Doesum, K. T. M., & Hoefnagels, C. (2010). Long-term effects of a home-visiting intervention for depressed mothers and their infants: Long-term effects of an early intervention. Journal of Child Psychology and Psychiatry, 51(10), 1160–1170. https://doi.org/10.1111/j.1469-7610.2010.02268.x
Kiani, M. A., Bahreyni Toosi, S. M. H., Badiei Aval, S., Gholian-avval, M., Zakerian, M., Hoseini, S. J., Peyman, N., Saberi, M. R., & Saeidi, M. (2021). Is home care a successful strategy in COVID-19? A valuable experience from Iran. International Journal of Pediatrics. https://doi.org/10.22038/ijp.2020.54311.4295
Kim, P. (2016). Human maternal brain plasticity: Adaptation to parenting. New Directions for Child and Adolescent Development, 2016(153), 47–58. https://doi.org/10.1002/cad.20168
Larkin, S. J., & Otis, M. (2019). The relationship of child temperament, maternal parenting stress, maternal child interaction and child health rating. Child and Adolescent Social Work Journal, 36(6), 631–640. https://doi.org/10.1007/s10560-018-0587-8
Liu, C.-C., Chen, Y.-C., Yeh, Y.-P., & Hsieh, Y.-S. (2012). Effects of maternal confidence and competence on maternal parenting stress in newborn care: Maternal confidence and competence. Journal of Advanced Nursing, 68(4), 908–918. https://doi.org/10.1111/j.1365-2648.2011.05796.x
Nygren, P., Green, B., Winters, K., & Rockhill, A. (2018). What’s happening during home visits? Exploring the relationship of home visiting content and dosage to parenting outcomes. Maternal and Child Health Journal, 22(S1), 52–61. https://doi.org/10.1007/s10995-018-2547-5
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M., & Picaza Gorrotxategi, M. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 Outbreak: An investigation in a sample of citizens in Northern Spain. Frontiers in Psychology, 11, 1491. https://doi.org/10.3389/fpsyg.2020.01491
Peacock, S., Konrad, S., Watson, E., Nickel, D., & Muhajarine, N. (2013). Effectiveness of home visiting programs on child outcomes: A systematic review. BMC Public Health, 13(1), 17. https://doi.org/10.1186/1471-2458-13-17
Pedrabissi, L., & Santinello, M. (1989). Inventario per l’ansia di «Stato» e di «Tratto»: nuova versione italiana dello STAI Forma Y: Manuale. Firenze: Organizzazioni Speciali, 44.
Phetrasuwan, S., & Shandor Miles, M. (2009). Parenting stress in mothers of children with autism spectrum disorders. Journal for Specialists in Pediatric Nursing, 14(3), 157–165. https://doi.org/10.1111/j.1744-6155.2009.00188.x
Pluess, M., & Belsky, J. (2011). Prenatal programming of post-natal plasticity? Development and Psychopathology, 23(1), 29–38. https://doi.org/10.1017/S0954579410000623
Provenzi, L., Grumi, S., Altieri, L., Bensi, G., Bertazzoli, E., Biasucci, G., Cavallini, A., Decembrino, L., Falcone, R., Freddi, A., Gardella, B., Giacchero, R., Giorda, R., Grossi, E., Guerini, P., Magnani, M. L., Martelli, P., Motta, M., Nacinovich, R., MOM-COPE Study Group. (2021). Prenatal maternal stress during the COVID-19 pandemic and infant regulatory capacity at 3 months: A longitudinal study. Development and Psychopathology. https://doi.org/10.1017/S0954579421000766
Provenzi, L., Grumi, S., Giorda, R., Biasucci, G., Bonini, R., Cavallini, A., Decembrino, L., Drera, B., Falcone, R., Fazzi, E., Gardella, B., Giacchero, R., Nacinovich, R., Pisoni, C., Prefumo, F., Scelsa, B., Spartà, M. V., Veggiotti, P., Orcesi, S., & Borgatti, R. (2020). Measuring the Outcomes of Maternal COVID-19-related Prenatal Exposure (MOM-COPE): Study protocol for a multicentric longitudinal project. British Medical Journal Open, 10(12), e044585. https://doi.org/10.1136/bmjopen-2020-044585
Provenzi, L., & Tronick, E. (2020). The power of disconnection during the COVID-19 emergency: From isolation to reparation. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S252–S254. https://doi.org/10.1037/tra0000619
Racine, S., Miller, A., Mehak, A., & Trolio, V. (2021). Examining risk and protective factors for psychological health during the COVID-19 pandemic. Anxiety, Stress, & Coping. https://doi.org/10.1080/10615806.2021.1958789
Reck, C., Hunt, A., Fuchs, T., Weiss, R., Noon, A., Moehler, E., Downing, G., Tronick, E. Z., & Mundt, C. (2004). Interactive regulation of affect in postpartum depressed mothers and their infants: An overview. Psychopathology, 37(6), 272–280. https://doi.org/10.1159/000081983
Rotheram-Borus, M. J., Tomlinson, M., le Roux, I. M., Harwood, J. M., Comulada, S., O’Connor, M. J., Weiss, R. E., & Worthman, C. M. (2014). A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. PLoS ONE, 9(10), e105934. https://doi.org/10.1371/journal.pone.0105934
Salehi, L., Rahimzadeh, M., Molaei, E., Zaheri, H., & Esmaelzadeh-Saeieh, S. (2020). The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: A structural equation model. Brain and Behavior. https://doi.org/10.1002/brb3.1835
Sheinkopf, S. J., Lester, B. M., LaGasse, L. L., Seifer, R., Bauer, C. R., Shankaran, S., Bada, H. S., Poole, W. K., & Wright, L. L. (2006). Interactions between maternal characteristics and neonatal behavior in the prediction of parenting stress and perception of infant temperament. Journal of Pediatric Psychology, 31(1), 27–40. https://doi.org/10.1093/jpepsy/jsj026
Spielberger, C. D. (1989). State-trait anxiety inventory: Bibliography. Consulting Psychologists Press.
Tchimtchoua Tamo, A. R. (2020). An analysis of mother stress before and during COVID-19 pandemic: The case of China. Health Care for Women International, 41(11–12), 1349–1362. https://doi.org/10.1080/07399332.2020.1841194
Vismara, L., Sechi, C., & Lucarelli, L. (2020). Reflective parenting home visiting program: A longitudinal study on the effects upon depression, anxiety and parenting stress in first-time mothers. Heliyon, 6(7), e04292. https://doi.org/10.1016/j.heliyon.2020.e04292
Williams, K., Ruiz, F., Hernandez, F., & Hancock, M. (2021). Home visiting: A lifeline for families during the COVID-19 pandemic. Archives of Psychiatric Nursing, 35(1), 129–133. https://doi.org/10.1016/j.apnu.2020.10.013
Acknowledgements
MOM-COPE Study Group: Lilia Altieri, Pietra Benedetta, Elisa Bettiga, Renza Bonini, Renato Borgatti, Anna Cavallini, Rossana Falcone, Elisa Fazzi, Barbara Gardella, Paola Guerini, Simona Orcesi, Dario Pantaleo, Federico Prefumo, Roberto Previtali, Laura Riva, Arsenio Spinillo, Patrizia Vergani, Maria Grazia Viganò
Funding
Open access funding provided by Università degli Studi di Pavia within the CRUI-CARE Agreement. This study is partially supported by the Italian Ministry of Health (Cinque per Mille, 2017) and Fondazione Roche Italia (Fondazione Roche per la Ricerca Indipendente) to author LP.
Author information
Authors and Affiliations
Consortia
Contributions
LP and RG: conceived the study; LP and SG: designed the methodology; RG, GB, LC, LD, MLM, MM, RN, PC, and BS: conducted data collection; ER: prepared the manuscript; LP and ER: finalized the submitted version of the manuscript; all authors agreed on the final manuscript version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors declares that they have no conflict of interest to disclose.
Ethical Approval
The study was approved by the Ethics Committee of Pavia (protocol ID: 20200037366; April 16th, 2020).
Consent to Participate
All participants provided informed consent prior to participation in the study.
Consent for Publication
No individual’s image was included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of MOM-COPE Study Group are listed in acknowledgements section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roberti, E., Giacchero, R., Grumi, S. et al. Post-partum Women’s Anxiety and Parenting Stress: Home-Visiting Protective Effect During the COVID-19 Pandemic. Matern Child Health J 26, 2308–2317 (2022). https://doi.org/10.1007/s10995-022-03540-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-022-03540-0