Abstract
Introduction
The aim of the present study was to compare clinical outcome between patients following fixed-bearing (FB) or mobile-bearing (MB) unicompartmental knee replacement (UKR) for antero-medial knee osteoarthrosis (OA) at two independent orthopedic centers.
Materials and methods
Matched-pairs were built between 35 patients receiving FB-UKR and 52 patients following MB-UKR regarding age at time of surgery, body mass index (BMI) and range of motion (ROM) preoperatively. Clinical and functional outcome was measured postoperatively by the American Knee Society Score (AKSS-O/AKSS-F), ROM, Tegner Activity Scale (TAS) as well as the Short Form 36 Health Survey (SF-36).
Results
The average treatment effect of the treated (ATT) after propensity score matching showed a significantly superior ROM in patients following MB-UKR (FB: 118°, MB: 124°). All remaining parameters had no statistically significant differences between both groups involving TAS, AKSS and SF-36.
Conclusions
The present study suggests that MB-UKR can provide a greater ROM compared to FB-UKR on comparable patients. The authors believe that both designs are suitable for adequate improvement of clinical outcome and ROM for patients suffering from antero-medial osteoarthrosis of the knee joint.
Level of evidence
Retrospective cohort study, Level IV.
Similar content being viewed by others
Introduction
Antero-medial knee osteoarthrosis (OA) can be treated either with total (TKR) or unicompartmental knee replacement (UKR). In approximately 50% of patients requiring knee arthroplasty, the criteria for using UKR are satisfied [1]. The usage of medial UKR has increased over the last decades with excellent outcomes in patient-reported outcome measures (PROMs) [2,3,4]. Major advantages of UKR compared to TKR comprises a significant lower rate of adverse events such as infections, blood loss or myocardial infarction [5]. Furthermore, patients following UKR tend to recover faster with shorter hospital stays and better range-of-motion (ROM) compared to patients following TKR [6].
Despite these advantages revision rates of UKR are up to five times higher than TKR, especially in registry-based studies [7, 8]. These differences in survival rates are often attributed to the surgeons learning curve. Liddle et al. showed that the revision rate in medial UKR diminishes with the increase in the number of UKRs performed by a single surgeon per year [5]. Still, these variation of survival rates between independent series, inventor studies and registries highlights the ongoing debate over which arthroplasty is superior.
In principle, there are two different implant design concepts for UKR. The first successful UKR used in 1969 was a fixed-bearing (FB) design with a flat all-polyethylene tibia [9]. To avoid high wear rates due to low conformity between articular surfaces, Goodfellow and O’Connor developed a prosthesis with a mobile-bearing design (MB) [10]. Since the early days of UKR, there has been a continuous improvement in MB- and FB-UKR to reduce design specific disadvantages which subsequently led to good clinical outcomes and survivorship with both implant designs [11, 12].
MB-UKR is designed to replicate tibiofemoral biomechanics better than FB-UKR [13, 14]. Furthermore, the higher conformity of the articular surfaces is considered to reduce contact stress and, therefore, minimize polyethylene wear [15,16,17]. On the other hand, there are studies which indicate the opposite regarding in vitro wear analyses with less wear rates in FB-UKR compared to MB-UKR [18, 19]. Bearing dislocation is a specific complication in MB-UKR which might lead to early failure of the implant. [20]. Some causes of dislocation are component malposition, release of the medial collateral ligament (MCL) or flexion–extension imbalance [21]. To decrease the risk of dislocation, surgeons tend to perform overcorrection to valgus to offload the medial compartment [22] which may lead to an increasing risk of progressive lateral compartment osteoarthritis [23], whereas an undercorrection of varus deformity is associated with a higher rate of bearing dislocation [24].
Conclusively surgeons need to follow a precise alignment and ligamentous balancing to reduce the risk of failure in MB-UKR, which indicates this design to be more prone to surgeon related errors. Therefore, the revision rate of MB-UKR correlates more with surgical experience and usage of UKR [5, 25, 26]. In FB-UKR the most common modes of failure are polyethylene wear and progressive OA in late years [24, 27].
Despite these differences in modes of failure and survivorship, a variety of studies suggesting similar functional outcomes between both designs [20, 27, 28]. Most of these publications did not consider preoperative parameters as a decisive part on postoperative functional outcome.
In this study we performed a matched-pairs analysis to compare clinical results in patients who underwent MB- or FB-UKR for antero-medial OA at two independent high-volume centers. Our hypothesis was that MB-UKR would be superior with respect to clinical parameters and range of motion (ROM).
Materials and methods
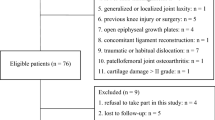
This matched-pair study is based on the retrospective analysis of prospectively collected data of a series of patients which underwent UKR for antero-medial OA in two different orthopedic centers. In total 272 UKR were analyzed subdivided into 35 FB-UKR implanted in the Department for Orthopaedics and Trauma of the University of Graz, Austria (Group A) and 237 MB-UKR implanted in the Center for Orthopaedics and Trauma Surgery of the University of Heidelberg, Germany (Group B). In group A, the Sigma® High Performance (HP) Partial Knee System (DePuy Synthes, Warsaw, IN) was used as FB-UKR and the Oxford Phase III Prosthesis (Biomet UK Limited, Swindon, UK) was used as MB-UKR in group B. In both centers, the primary indication was advanced osteoarthritis of the medial compartment with full-thickness articular cartilage loss or avascular necrosis of the medial femoral condyle. In all cases, the anterior cruciate ligament (ACL) as well as the medial (MCL) and lateral (LCL) collateral ligaments were functionally intact, the varus deformity was manually correctable at 20° flexion and there was no evidence of osteoarthritis in the lateral compartment on valgus stress radiographs. Osteoarthritis of the patellofemoral joint was not considered to be a contraindication unless there was deep eburnation or bone grooving on the medial facet of the patella.
In both centers, all surgeries were performed using the minimally invasive surgical technique through a medial parapatellar approach without dislocation of the patella. Whereas, all FB-UKR were implanted with cemented fixation, MB-UKR were implanted with cemented or uncemented fixation depended on the bone quality. An intravenous single-shot antibiotic (1.5 g cefuroxime) was administered perioperatively. Immediate full weight bearing was allowed postoperatively.
At the last follow-up, the clinical outcome was evaluated using the American Knee Society Scores (AKSS-F and AKSS-O) [29] as well as the range of motion (ROM). ROM was objectified by goniometer pre- and postoperatively. Postoperative activity level was assessed using the Tegner Activity Scale (TAS) [30]. The state of general health was assessed using the Short Form 36 Health Survey (SF-36), which is a widely used assessment due its reliability and validity [31, 32].
Statistical methods
All data were analysed by Stata Version 17 (Stata Corp LLC, Texas, USA).
Means and medians are provided with corresponding standard deviations and interquartile ranges for normally and non-normally distributed variables, respectively. Propensity score matching using the Stata add-on psmatch2 was used to account for imbalances between the two cohorts. A propensity score (PS) was calculated based on patient age at time of surgery, body mass index (BMI), and ROM of the affected joint at time of surgery. Nearest neighbour-matching with 3 neighbours was used to calculate the matched outcome was applied. Balancing of variables between matched cohorts was assessed with Stata add-on pstest. Remaining bias of < 5% was considered as sufficient balancing. The average treatment effect of the treated (ATT) was assessed for specific outcome variables on the matched and PS-weighted cohort. A p value of < 0.05 was considered statistically significant.
An a priori power analysis according to the magnitude of a 10% difference for the endpoints AKSS-F, AKSS-O and ROM was performed with a p value < 0.05 and a power greater than 80%, which revealed a minimum number of n = 35 cases per group as sufficient. Matching was performed with respect to age, BMI, and preoperative ROM in a 1:1.5 ratio and the maximum caliper set at 0.2.
Results
We were able to match 35 patients following FB-UKR (Group A) with 52 patients following MB-UKR (Group B) regarding parameters age at time of surgery, BMI and ROM preoperatively. Hereby, we eradicated significant differences between both groups preoperatively in those mentioned parameters after Propensity-Score matching (p > 0.05, Table 1).
The matched pairs are well balanced in age (bias − 2.5%) and BMI (bias − 1.7%) such as moderate balanced in ROM preoperatively (bias − 22.0%). Patient demographic data are shown in Table 2.
The ATT after propensity score matching showed a significantly superior postoperative ROM in Group B (FB: 118.43, MB: 124.86, t-score: − 2.55). All remaining parameters had no statistically significant differences between groups involving TAS (FB: 3.97, MB: 3.62, t-score: 1.46), SF-36 items function (FB: 85.71, BB: 77.38, t-score: 1.77), role function (FB: 78.75, MB 75.24, t-score: 0.44), pain (FB: 78.00, MB: 75.24, t-score: 0.24), condition (FB: 71.54, MB: 67.10, t-score: 0.88), vitality (FB: 68.21, MB: 66.90, t-score: 0.29), social function (FB: 91.07, MB: 88.45, t-score: 0.60), emotional (FB: 83.57, MB: 84.44, t-score: − 0.12), psychologic (FB: 77.29, MB: 81.71, t-score: − 1.12), such as AKSS-F (FB: 93.14, MB: 89.19, t-score: 1.19). The AKSS-O was slightly better in group A (FB: 96.86, MB: 91.84, t-score: 1.90). All details are given in Table 3.
Discussion
The aim of our study was to compare clinical outcome parameters of patients following MB-UKR and FB-UKR for antero-medial OA in a matched pairs two center study. Our hypothesis was that MB-UKR would be superior with respect to clinical parameters and ROM.
The most important finding of the study is that ROM after MB-UKR seems to be significantly superior than after FB-UKR. As our patients were matched regarding age, BMI and preoperative ROM, it is assumable that there was no influence on differences regarding the clinical outcome between both groups by these parameters.
While many studies analyzed survivorship of FB- and MB-UKR and only reported second about functional outcome parameters, this present study focused primary on the clinical outcome of those designs [17, 20, 27, 28]. Interestingly to date there are only 3 randomized control trials (RCT) comparing outcome parameters of both implant designs [33,34,35]. While two are outdated [34, 35], the remaining study compared a robotic-assisted procedure in FB-UKR with a conventional implantation of MB-UKR [33], which might influence the postoperative functional outcome parameters regardless the used implant design. Despite these studies, the mentioned publication were mostly systematic analyses comparing functional outcome parameters between both implant designs without taking the preoperative status into account. In contrast to this, our patients were matched by the preoperative knee function, which is a strength of the current study.
Gleeson et al. reported about no differences in ROM after MB-UKR and FB-UKR as did Li et al. comparing the Miller-Galante Unicompartmental Knee (FB-UKR) with the Oxford UKA (MB-UKR) [35, 36]. Furthermore, Parratte et al. compared 79 FB-UKR with 77 MB-UKR demonstrating no statistically significant differences regarding postoperative ROM in both groups [37]. To our knowledge, the present study is the first matched-pair analysis between FB-UKR and MB-UKR using preoperative ROM as a matching parameter to exclude any influence on the postoperative outcome by this parameter. Therefore, we suggest MB-UKR can provide a greater ROM than FB-UKR considering the preoperative ROM. This might be explained by a more physiologically joint kinematic after MB-UKR as reported by Li et al. [14, 38]. Nevertheless, the clinical benefit of the superior ROM remains unsure as it is not reflected in the functional outcome and activity level in our cohorts.
There was no statistically significant difference in the postoperative AKSS between both groups, while both achieving excellent results comparable to other studies [20, 39,40,41].
The current literature supports the hypothesis that clinical results following FB-UKR and MB-UKR are comparable and do not differ significantly. A systematic review by Peersman et al. analyzing 44 studies reported similar AKSS-O/ AKSS-F Scores after 5 years for FB-(88.2/86.4) and MB-UKR (88.1/85.7)[20]. A randomized prospective study comparing both designs demonstrated good to excellent clinical results regarding the AKSS without differences between them [36]. Supporting these findings Smith et al. found no differences between FB- and MB-UKR groups regarding the Bristol Knee Score, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, Oxford Knee Score (OKS) and AKSS in their systematic analysis [28].
Since the usage of UKR increased in the last decade, consequently more young and active patients are treated with UKR [42, 43]. As clinical results are not always conclusive with the actual activity level of the patient [44], it is helpful to use activity rating scales such as the TAS additionally. Earlier studies have shown that patients following FB- and MB-UKR can restore their activity level, especially in low impact sports such as hiking, swimming and cycling [11, 45,46,47]. While several studies reported differences in postoperative activity levels between patients following TKR and UKR, there are no studies that have shown such differences between patients following FB- and MB-UKR [8, 45, 48, 49]. In our study, there was no difference in postoperative activity level measured by TAS between Group A (3.97) and Group B (3.62), which supports the hypothesis that both implant designs can provide a moderate level of activity postoperatively.
Regarding the general state of health of patients following UKR, Pronk et al. have shown similar results for both implant designs assessed by the 3-level version of EuroQol 5 Dimensions [50]. Li et al. reported a significant improvement of quality of life measured by the SF-36 Score from preoperative to 2 years postoperatively in 28 FB- and 28 MB-UKR without any difference between the groups [36]. Consistent with that, Neufeld et al. have shown no statistically significant difference after a 10 year follow-up regarding the SF12-Score between patients following FB- and MB-UKR [40]. Our matched-pairs analysis fits in the current literature as it showed no significant differences in the general state of health between both groups measured by the SF-36 Score.
There are several limitations to this study such as the limited sample size especially in the FB-group as well as the retrospective study design. In addition, functional outcome parameters were only assessed postoperative. Therefore, a comparison between changes from preoperative to postoperative were not possible.
Since the ROM was assessed with a goniometer by many different examiners, there could be a higher interobserver variability in our study design. Accordingly, the shown differences in ROM between both groups need to be carefully interpreted. Even though the ROM may differ statistically significant, the authors believe it is not relevant in this extent regarding patient benefits.
In addition, two different systems implanted by different surgeons were evaluated in this analysis. However, both systems are only available in the used designs, and therefore, a comparison between different developers is inevitable to analyze design specific differences. Due to a matched-pair and propensity score analysis, we could further minimize this bias.
Conclusions
This matched-pairs analysis showed a significantly superior ROM after MB-UKR compared with FB-UKR, while there were no significant differences in AKSS, TAS and SF-36. The authors believe that both designs are suitable for adequate improvement of clinical outcome and ROM for patients suffering from antero-medial osteoarthritis of the knee joint.
Data availability
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- AKSS:
-
American knee society score
- ATT:
-
Average treatment effect of the treated
- BMI:
-
Body mass index
- FB:
-
Fixed-bearing
- LCL:
-
Lateral collateral ligament
- MB:
-
Mobile-bearing
- MCL:
-
Medial collateral ligament
- OA:
-
Osteoarthrosis
- OKS:
-
Oxford knee score
- PROMs:
-
Patient-reported outcome measures
- RCT:
-
Randomized control trials
- ROM:
-
Range of motion
- SF-36:
-
Short Form 36 Health Survey
- TAS:
-
Tegner Activity Scale
- TKR:
-
Total knee replacement
- UKR:
-
Unicompartmental knee replacement
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
References
Murray DW, Parkinson RW (2018) Usage of unicompartmental knee arthroplasty. Bone Jt J 100-B(4):432–5. https://doi.org/10.1302/0301-620X.100B4.BJJ-2017-0716.R1
Hefny MH, Smith NA, Waite J (2020) Cementless medial Oxford unicompartmental knee replacement. Five-year results from an independent series. Knee 27(4):1219–27. https://doi.org/10.1016/j.knee.2020.05.009
Mohammad HR, Kennedy JA, Mellon SJ, Judge A, Dodd CA, Murray DW (2020) Ten-year clinical and radiographic results of 1000 cementless Oxford unicompartmental knee replacements. Knee Surg Sports Traumatol Arthrosc 28(5):1479–1487. https://doi.org/10.1007/s00167-019-05544-w
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Jt Surg Br 93(2):198–204. https://doi.org/10.1302/0301-620X.93B2.25767
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384(9952):1437–1445. https://doi.org/10.1016/S0140-6736(14)60419-0
Lombardi AV Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467(6):1450–1457. https://doi.org/10.1007/s11999-009-0731-z
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25(5):799–806. https://doi.org/10.1007/s00590-015-1610-9
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822. https://doi.org/10.1007/s00167-017-4817-y
Engelbrecht E, Siegel A, Rottger J, Buchholz HW (1976) Statistics of total knee replacement: partial and total knee replacement, design St. Georg: a review of a 4-year observation. Clin Orthop Relat Res 120:54–64
Goodfellow J, O’Connor J (1978) The mechanics of the knee and prosthesis design. J Bone Jt Surg Br 60-B(3):358–69
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Jt J 97-B(11):1493–500. https://doi.org/10.1302/0301-620X.97B11.35634
Song SJ, Bae DK, Kim KI, Park CH (2019) Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surg Sports Traumatol Arthrosc 27(4):1310–1319. https://doi.org/10.1007/s00167-019-05390-w
Choy WS, Lee KW, Kim HY, Kim KJ, Chun YS, Yang DS (2017) Mobile bearing medial unicompartmental knee arthroplasty in patients whose lifestyles involve high degrees of knee flexion: a 10–14year follow-up study. Knee 24(4):829–836. https://doi.org/10.1016/j.knee.2017.05.004
Mullaji AB, Shah S, Shetty GM (2017) Mobile-bearing medial unicompartmental knee arthroplasty restores limb alignment comparable to that of the unaffected contralateral limb. Acta Orthop 88(1):70–74. https://doi.org/10.1080/17453674.2016.1253327
Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM (2002) Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Jt Surg Am 84(12):2235–2239
Emerson RH Jr, Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70. https://doi.org/10.1097/01.blo.0000036525.46246.b7
Whittaker JP, Naudie DD, McAuley JP, McCalden RW, MacDonald SJ, Bourne RB (2010) Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin Orthop Relat Res 468(1):73–81. https://doi.org/10.1007/s11999-009-0975-7
Burton A, Williams S, Brockett CL, Fisher J (2012) In vitro comparison of fixed- and mobile meniscal-bearing unicondylar knee arthroplasties: effect of design, kinematics, and condylar liftoff. J Arthroplasty 27(8):1452–1459. https://doi.org/10.1016/j.arth.2012.02.011
Brockett CL, Jennings LM, Fisher J (2011) The wear of fixed and mobile bearing unicompartmental knee replacements. Proc Inst Mech Eng H 225(5):511–519. https://doi.org/10.1177/2041303310393824
Peersman G, Stuyts B, Vandenlangenbergh T, Cartier P, Fennema P (2015) Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 23(11):3296–3305. https://doi.org/10.1007/s00167-014-3131-1
Huang F, Wu D, Chang J, Zhang C, Qin K, Liao F et al (2021) A Comparison of mobile- and fixed-bearing unicompartmental knee arthroplasties in the treatment of medial knee osteoarthritis: a systematic review and meta-analysis of 1,861 Patients. J Knee Surg 34(4):434–443. https://doi.org/10.1055/s-0039-1697901
Peersman G, Slane J, Vuylsteke P, Fuchs-Winkelmann S, Dworschak P, Heyse T et al (2017) Kinematics of mobile-bearing unicompartmental knee arthroplasty compared to native: results from an in vitro study. Arch Orthop Trauma Surg 137(11):1557–1563. https://doi.org/10.1007/s00402-017-2794-8
Ko YB, Gujarathi MR, Oh KJ (2015) Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications. Knee Surg Relat Res 27(3):141–148. https://doi.org/10.5792/ksrr.2015.27.3.141
van der List JP, Zuiderbaan HA, Pearle AD (2016) Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty 31(5):1016–1021. https://doi.org/10.1016/j.arth.2015.11.030
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Jt Surg Br 83(1):45–49. https://doi.org/10.1302/0301-620x.83b1.10871
Liddle AD, Pandit H, Judge A, Murray DW (2016) Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Jt Surg Am 98(1):1–8. https://doi.org/10.2106/JBJS.N.00487
Abu Al-Rub Z, Lamb JN, West RM, Yang X, Hu Y, Pandit HG (2020) Survivorship of fixed vs mobile bearing unicompartmental knee replacement: a systematic review and meta-analysis of sixty-four studies and National Joint Registries. Knee 27(5):1635–1644. https://doi.org/10.1016/j.knee.2020.09.004
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605. https://doi.org/10.1016/j.otsr.2009.10.006
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Briggs KK, Steadman JR, Hay CJ, Hines SL (2009) Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med 37(5):898–901. https://doi.org/10.1177/0363546508330149
Laucis NC, Hays RD, Bhattacharyya T (2015) Scoring the SF-36 in orthopaedics: a brief guide. J Bone Jt Surg Am 97(19):1628–1634. https://doi.org/10.2106/JBJS.O.00030
Schleiter MK, Tarlov AR (1983) National study of Internal Medicine Manpower: VIII. Internal medicine residency and fellowship training: 1983 update. Ann Intern Med 99(3):380–7
Gilmour A, MacLean AD, Rowe PJ, Banger MS, Donnelly I, Jones BG et al (2018) Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty the 2-year clinical outcomes of a randomized controlled trial. J Arthroplasty 33(7S):S109–S15. https://doi.org/10.1016/j.arth.2018.02.050
Confalonieri N, Manzotti A, Pullen C (2004) Comparison of a mobile with a fixed tibial bearing unicompartimental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee 11(5):357–362. https://doi.org/10.1016/j.knee.2004.01.003
Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH (2004) Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee 11(5):379–384. https://doi.org/10.1016/j.knee.2004.06.006
Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13(5):365–70. https://doi.org/10.1016/j.knee.2006.05.003
Parratte S, Pauly V, Aubaniac JM, Argenson JN (2012) No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res 470(1):61–68. https://doi.org/10.1007/s11999-011-1961-4
Li M, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile vs fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13:365–70
Smith JR, Robinson JR, Porteous AJ, Murray JR, Hassaballa MA, Artz N et al (2014) Fixed bearing lateral unicompartmental knee arthroplasty–short to midterm survivorship and knee scores for 101 prostheses. Knee 21(4):843–847. https://doi.org/10.1016/j.knee.2014.04.003
Neufeld ME, Albers A, Greidanus NV, Garbuz DS, Masri BA (2018) A Comparison of mobile and fixed-bearing unicompartmental knee arthroplasty at a minimum 10-year follow-up. J Arthroplasty 33(6):1713–1718. https://doi.org/10.1016/j.arth.2018.01.001
Cao Z, Niu C, Gong C, Sun Y, Xie J, Song Y (2019) Comparison of fixed-bearing and mobile-bearing unicompartmental knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 34(12):3114–23.e3. https://doi.org/10.1016/j.arth.2019.07.005
Biswas D, Van Thiel GS, Wetters NG, Pack BJ, Berger RA, Della Valle CJ (2014) Medial unicompartmental knee arthroplasty in patients less than 55 years old: minimum of two years of follow-up. J Arthroplasty 29(1):101–105. https://doi.org/10.1016/j.arth.2013.04.046
Bruni D, Akkawi I, Iacono F, Raspugli GF, Gagliardi M, Nitri M et al (2013) Minimum thickness of all-poly tibial component unicompartmental knee arthroplasty in patients younger than 60 years does not increase revision rate for aseptic loosening. Knee Surg Sports Traumatol Arthrosc 21(11):2462–2467. https://doi.org/10.1007/s00167-013-2578-9
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplasty 13(8):890–895
Papalia R, Zampogna B, Torre G, Diaz Balzani LA, Vasta S, Papalia G et al (2020) Return to sport activity in the elderly patients after unicompartmental knee arthroplasty: a systematic review and meta-analysis. J Clin Med. https://doi.org/10.3390/jcm9061756
Waldstein W, Kolbitsch P, Koller U, Boettner F, Windhager R (2017) Sport and physical activity following unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 25(3):717–728. https://doi.org/10.1007/s00167-016-4167-1
Walker T, Streit J, Gotterbarm T, Bruckner T, Merle C, Streit MR (2015) Sports, physical activity and patient-reported outcomes after medial unicompartmental knee arthroplasty in young patients. J Arthroplasty 30(11):1911–1916. https://doi.org/10.1016/j.arth.2015.05.031
Witjes S, Gouttebarge V, Kuijer PP, van Geenen RC, Poolman RW, Kerkhoffs GM (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med 46(2):269–292. https://doi.org/10.1007/s40279-015-0421-9
Hopper GP, Leach WJ (2008) Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc 16(10):973–979. https://doi.org/10.1007/s00167-008-0596-9
Pronk Y, Paters AAM, Brinkman JM (2021) No difference in patient satisfaction after mobile bearing or fixed bearing medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 29(3):947–954. https://doi.org/10.1007/s00167-020-06053-x
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MH, TW, GH, MS, PS, BP and TR. The first draft of the manuscript was written by MH, TW and PS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The Author TR has received research support and personal fees from Arbeitsgemeinschaft Endoprothetik (AE), DGOU, DGOOC, BVOU, DePuy International, Otoo Bock Foundation, Deutsche Arthrose Hilfe, Aesculap, Zimmer, Stiftung Oskar Helene Heim Berlin, Vielberth Foundation Regensburg, the German Ministry of Education and Research as well as the German Federal Ministry of Economic Cooperation and Development. The Author BP has received institutional grants from Zimmer Biomet. The Author CM has received institutional financial support from Zimmer Biomet, Medacta, Depuy and Johnson & Johnson not directly related to this study. Furthermore, he has received author payments from Thieme. The Author AL has received institutional grants from Medtronic, Alphamed and Johnson & Johnson not directly related to this study. The other authors declare that they have no competing interests.
Ethical approval
Ethical approval was obtained by the institutional review boards of the University of Heidelberg and University of Graz. The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013.
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of their individual data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hariri, M., Hauer, G., Smolle, M. et al. Mobile bearing versus fixed bearing medial unicompartmental knee replacement: an independent two center matched-pairs analysis. Arch Orthop Trauma Surg 143, 3383–3389 (2023). https://doi.org/10.1007/s00402-022-04629-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04629-5