Abstract
Summary
In this prospective study in Swedish elderly men, PAD based on an ABI < 0.9 was associated with an increased risk of hip fracture, independent of age and hip BMD. However, after further adjustments for comorbidity, medications, physical function, and socioeconomic factors, the association diminished and was no longer statistically significant.
Introduction
To examine if peripheral arterial disease (PAD) is associated with an increased risk for hip fracture in men independent of hip BMD.
Methods
Ankle-brachial index (ABI) was assessed in the Swedish MrOS (Osteoporotic Fractures in Men) study, a prospective observational study including 3014 men aged 69–81 years at baseline. PAD was defined as ABI < 0.90. Incident fractures were assessed in computerized X-ray archives. The risk for hip fractures was calculated using Cox proportional hazard models. At baseline, BMD was assessed using DXA (Lunar Prodigy and Hologic QDR 4500) and functional measurements and blood samples were collected. Standardized questionnaires were used to collect information about medical history, falls, and medication.
Results
During 10 years of follow-up, 186 men had an incident hip fracture. The hazard ratio (HR) for hip fracture in men with PAD was 1.70 (95% CI 1.14–2.54), adjusted for age and study site. Additional adjustment for total hip BMD marginally affected this association (HR 1.64; 95% CI 1.10–2.45). In a final multivariate model, the HR attenuated to a non-significant HR 1.38 (95% CI 0.91–2.11) adjusted for age, site, hip BMD, BMI, falls, smoking, eGFR, handgrip strength, walking speed, former hip fracture, antihypertensive treatment, diabetes, education, and history of cardiovascular disease.
Conclusion
This study suggests that PAD is associated with an increased risk for hip fracture independently of hip BMD in elderly Swedish men. However, the high frequency of comorbidity and lower physical performance among men with PAD might partly explain this association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several observational studies support an association between cardiovascular disease and osteoporotic fracture risk [1]. However, the evidence for associations between peripheral arterial disease (PAD) and fracture risk is limited. PAD, referred to as the atherosclerotic occlusive disease of the lower extremities, is closely related to generalized atherosclerosis and associated with a significantly increased risk for cardiovascular events [2]. In addition, PAD shares several risk factors with fragility fractures, particularly hip fractures. Like hip fractures, PAD has a sharply increasing prevalence with older age, reaching almost 20% by the age of 80 [2, 3]. PAD limits lower limb function and has been associated with impaired balance [4,5,6]. Also, lifestyle risk factors and comorbidity are shared. The Hong Kong MrOS study showed that smoking is a risk factor for both PAD and low bone mineral density (BMD) [7], and diabetes is well known to be associated with both atherosclerotic diseases [8] and increased risk for fractures [9]. Accordingly, it is reasonable to suspect that individuals with PAD have an altered risk for incident fractures.
Hip fractures are frequently regarded as the most harmful fracture in the elderly, associated with high mortality and loss of function [10]. Low BMD is a strong risk factor for fractures in the elderly [11]. Associations between modestly reduced BMD and subclinical as well as clinical atherosclerotic conditions have been found, such as aortic calcification, carotid artery calcification, and coronary artery disease [1, 12, 13]. A few studies have also specifically reported an association between PAD and reduced BMD [14,15,16], but conflicting results exist [17, 18]. The US MrOS study showed that men with PAD had lower BMD and increased risk for incident non-vertebral fractures, but not for hip fractures [16]. In contrast, some larger cohort studies have reported significant associations between PAD and increased risk of hip fracture in both men and women, as compared to individuals without PAD [19,20,21]. However, the lack of adjustments for factors such as BMD, body mass index (BMI), and falls, limits the understanding of mechanisms underpinning the association. In other studies that adjusted for these factors, no significant association between PAD and hip fracture risk was observed, but then with lack of power due to small study samples or shorter follow-up time [16, 22, 23]. Overall, the number of previous studies is still limited, and the results are somewhat inconsistent. Therefore, we sought to test the hypothesis that PAD is associated with increased hip fracture risk in elderly men. Furthermore, we aimed to investigate whether potential associations were independent of age, BMD, BMI, and other possible confounders and mediating factors including comorbidity, socioeconomic factors, and physical function. As secondary outcomes, other fracture types were investigated.
Method
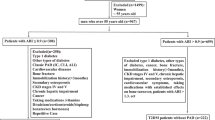
Study sample
The Osteoporotic Fractures in Men (MrOS) study is a prospective, multicentre observational study, conducted with the main aim to identify risk factors for osteoporosis and fractures in men. MrOS comprises elderly men in the USA (n = 5994), Sweden (n = 3014), and Hong Kong (n = 2000). In this study, the MrOS Sweden cohort was used to assess associations between PAD and hip fracture risk.
The MrOS Sweden cohort consists of sub-cohorts from three cities in Sweden (Gothenburg n = 1010, Malmö n = 1005, and Uppsala n = 999). Men at 69–81 years of age were randomly identified from national population registries and invited by letter to participate during the years 2001–2004. To be eligible for the study, the participants had to be able to walk without assistance, not have bilateral hip prostheses, and the capability to answer questionnaires in Swedish on their own. The attendance rate was 45%. At baseline, the participants were examined, answered questionnaires, underwent blood sampling, and were measured for BMD. Written informed consent was obtained from all study participants. The ethics committees at the Universities of Gothenburg, Lund, and Uppsala approved the study.
Assessment of peripheral arterial disease (PAD)
Ankle-brachial index (ABI) was measured at baseline by specifically trained staff. Systolic blood pressure was measured twice in the right arm in a seated position after 10 min of rest, and twice from the posterior tibial artery of each ankle. The dorsalis pedis artery pressure was used if a posterior tibial signal was not audible, and the left arm was used if the right arm was not appropriate. To determine ABI, the average of the two readings of the ankle systolic pressure was divided by the average of the two brachial artery systolic pressures. PAD was defined as ABI < 0.90 in one or both legs. Subjects with an ABI > 1.40 were excluded (28 cases), as it might represent falsely high values due to incompressible arteries. Further details of the ABI-measurement procedure have been described previously [24].
Assessment of covariates
A standardized questionnaire was used to collect information about previous fractures, smoking habits, alcohol use, and falls (yes/no) during the last 12 months preceding the baseline visit. Also, self-reported prevalent diseases were assessed. Current medicine use was assessed by interview or by the delivery of packages of ongoing medications, including both prescribed and over-the-counter drugs. All medications were registered according to the Anatomical Therapeutic Chemical (ATC) Classification System. Body height and weight were measured using standard equipment, of which body mass index (BMI) was calculated (kg/m2). Muscle strength was estimated by measurement of handgrip strength, using a Jamar® hand dynamometer (Jackson, MI, USA). The best value from four measurements (two of each hand) was used. Walking speed was estimated by the duration (seconds) of a 6-m walk at a normal pace. The test was performed two times and the fastest performance was analyzed. BMD at hip sites and lumbar spine, as well as lean and fat mass, were assessed using dual-energy X-ray absorptiometry (DXA). The Hologic QDR 4500/A-Delphi (Hologic, Waltham, MA, USA) was used in Gothenburg, and the Lunar Prodigy DXA (GE Lunar Corp., Madison, WI, USA) was used in Lund and Uppsala. As the DXA measurement was performed with equipment from different manufacturers, standardized BMD was calculated. Blood samples were collected at 8:00 a.m. after an overnight fast and non-smoking, frozen within 1 h, and stored at –80 °C until required for analysis. Glomerular filtration rate (GFR) was calculated with serum cystatin C. High-sensitive CRP (hsCRP) was measured by an ultrasensitive particle‐enhanced immunoturbidimetric assay and the specific method has been described previously [25].
Assessment of hip fractures and follow-up time
Fracture outcomes were collected after the baseline visit until December 31, 2012. All incident fractures were identified by reviewing computerized X-ray archives in Gothenburg, Lund, and Uppsala, using the unique personal registration number assigned to all Swedish citizens. Thus, only fractures confirmed by radiology were included, and only the first fracture of each location during follow-up was considered. The main outcome is hip fracture, but also all incident fractures, major osteoporotic fractures (including fractures of the hip, vertebrae, forearm, and humerus), and nonvertebral osteoporotic fractures (comprising hip, pelvis, proximal humerus, and forearm fractures) are assessed.
Participants were followed until the date of their first hip fracture, death, or the end of year 2012. The date of death was retrieved from the National Cause of Death Register, comprising more than 99% of all deaths in Sweden. In total, 1246 men died during the study (41%). The median follow-up time was 10 years.
Statistical analyses
Data are presented as proportions (%) or absolute numbers (n), or means with standard deviations (SD), as appropriate. Differences in means between two groups regarding baseline data were tested with a double-sided t-test if the dependent variable was either ordinal or continuous. The test of O’Brien was used to test whether both groups had equal mean and variance. If data were skewed, the non-parametric Mann–Whitney U test was used. A p-value < 0.05 was considered statistically significant. Some measurements were only obtained in the Gothenburg part of MrOS (one-third of the study sample) and are presented separately.
The risk for hip fractures was calculated using Cox proportional hazard models and the hazard ratios (HR) are presented with 95% confidence intervals (CI). The Schoenfeld Residuals Test was performed to ascertain the model assumption of proportional hazard. Since we expected men with PAD to have a higher degree of overall morbidity and higher risk of death, the Cox models were assured to censor for events of death in accordance with a cause specific hazard model [26], and by such considering death as a competing risk factor.
Possible confounding factors were included in multivariate Cox models, based on the assumption of being causally related to the outcome (fracture) as well as associated with the exposure (PAD), but not an obvious mediating factor in the potential association between the exposure and the outcome. Thus, we included established risk factors for hip fractures that also empirically have been associated with PAD or were unequally distributed between men with and without PAD in the present cohort, comprising hip BMD, BMI, current smoking, eGFR, antihypertensive treatment, diabetes, former hip fracture, and prevalent cardiovascular diseases at baseline. In addition, we included some variables that probably rather serve as mediating factors in the causal chain between PAD and fracture outcomes; falls, handgrip strength (as a measurement of muscle strength), and walking speed (as a measurement of physical performance). Notably, such factors could potentially serve as both confounders and mediating factors, which is discussed further during the discussion part of this paper. Moreover, we also left out some potentially relevant confounders to avoid multicollinearity or overadjustment [27], with the motivation that they theoretically significantly correlate (represent much of the same phenomenon) with any of the already included variables. In these cases, we chose to include the variable that we biologically or clinically found most relevant. Current smoking was included as a covariate but not chronic obstructive pulmonary disease (COPD), with the motivation that smoking is the main cause of COPD and a strong risk factor for fractures on its own, and alcohol use was left out since we included previous falls. Handgrip strength was included as it represents the primary parameter of sarcopenia and is regarded as the most reliable measure of muscle strength [28], whereas appendicular lean mass was left out due to its correlation to handgrip strength (r = 34 when tested in a correlation analysis). None of the factors collected only in the Gothenburg cohort was used in the Cox models due to the limited sample size.
Eligible covariates were forward included one by one in the Cox proportional hazard models. First, the Cox models were adjusted for age and study site and separately for each covariate of interest, in order to identify any specific factor that most prominently would impact the association between PAD and hip fracture risk. Then, multivariate models including several assumed confounders were conducted, and separate multivariate models including assumed mediating factors, with an ultimate final model including both. All analyses were made using Stata for Windows, version 15 (Stata Corp, TX 77,845, USA), and a statistics program package developed at the Department of Community Medicine and Public Health, Gothenburg University.
Results
At baseline, 2893 men had an ABI measurement, and PAD was found in 10.9% (314 men). During follow-up, 186 men experienced an incident hip fracture, of which 29 had PAD at baseline. Baseline characteristics according to PAD status are shown in Tables 1 and 2. Men with PAD were older and had lower lean mass and lower BMD at hip sites. However, BMI and fat mass did not significantly differ from men without PAD. As expected, men with PAD were more often current smokers and had more comorbidity such as COPD, diabetes, hypertension, and additional manifestations of cardiovascular diseases. Estimated GFR (eGFR) was also lower in men with PAD. The number of falls tended to be higher in men with PAD (p = 0.09). In line with increased morbidity, men with PAD also had lower educational level. Results from the Gothenburg part of the MrOS study indicated higher serum cortisol level and higher urinary cadmium level in men with PAD (Table 2). Both handgrip strength and walking speed were poorer among men with PAD. Severe sarcopenia defined by EWGSOP2 was uncommon (handgrip strength < 27 kg together with appendicular lean mass < 7 kg/m2 and 6 m walking speed < 1 m/s) [28], but yet overrepresented among men with PAD (Table 3). These results are cross-sectional and not adjusted for the difference in age between exposure groups, but an interaction model showed no statistically significant interaction between muscle measurements and age. Mortality during the follow-up time was higher in men with PAD versus men without PAD, with an age-adjusted HR of 2.05 (95% CI 1.77–2.39).
PAD at baseline was associated with an increased risk of hip fracture as compared to men without PAD (HR 1.70; 95% CI 1.14–2.54), adjusted for age and study site (Table 4). Additional adjustment for total hip BMD only marginally affected this association (HR 1.67; 95% CI 1.12–2.48). None of the assessed confounding or mediating factors solely attenuated the association between PAD and hip fracture risk to a non-significant level, except for the variable walking speed. However, in the multivariate models including several confounding and mediating factors, the HR for hip fracture in men with PAD further weakened to a non-significant level, with a HR 1.38 (95% CI 0.91–2.11) in the final model adjusted for age, site, hip BMD, BMI, falls, current smoking, eGFR, handgrip strength, walking speed, former hip fracture, antihypertensive treatment, diabetes, level of education, and history of cardiovascular disease. Our power was too limited to investigate the severity of PAD for fracture risk, but a sub-analysis showed an almost threefold increased risk for hip fracture in men with ABI < 0.5 as compared to men without PAD (HR 2.83; 95% CI 1.05–7.62), adjusted for age, study site and hip BMD. However, this estimate should be interpreted with caution since only 25 men had an ABI < 0.5.
In addition, the association between PAD at baseline and other fracture outcomes was analyzed (Table 5). PAD was associated with an increased risk for all fractures (HR 1.35; 95% CI, 1.07–1.70) as well as major osteoporotic fractures (HR 1.43; 95% CI, 1.09–1.86) adjusted for age, site, and hip BMD. But in the final multivariate models, the results were non-significant (1.17; 95% CI, 0.92–1.49, and 1.24; 95% CI, 0.94–1.65, respectively). None-vertebral osteoporotic fractures were significantly associated with an increased fracture risk only in the crude model adjusted for age and study site, while no significant association between PAD and vertebral fractures was seen. A full overview of the stepwise inclusion of covariates in the multivariate models for hip fractures as well as other fracture outcomes is illustrated in the supplementary Table 6.
Discussion
In this prospective study in Swedish elderly men, we found PAD based on an ABI < 0.9 to be associated with an increased risk of hip fracture independent of age and hip BMD (HR 1.67; 95% CI 1.12–2.48). But after further adjustments for comorbidity, medications, physical function, and educational level, the association attenuated and was no longer statistically significant.
Prior studies — similarities and differences
In this section, we dive deeper into prior studies investigating the association between PAD and hip fracture risk. The aim is to highlight strengths and weaknesses as well as differences compared to the present study that might explain some of the inconsistent results.
First, a population-based cohort study from Australia including 4321 men reported an increased risk for hip fracture in men with PAD compared to men without PAD (HR 1.69; 95% CI 1.08–2.63) [20], independent of age, BMI, smoking, alcohol consumption, previous stroke, coronary heart disease, and abdominal aortic aneurysm. A large register-based cohort study from Taiwan including 1464 incident hip fractures showed similar results with HR 1.57 (95% CI 1.45–1.71) for hip fractures in women with PAD, and HR 1.50 (95% CI 1.44–1.78) for men with PAD, independent of age-group, income, numerous medical conditions, and medications [21]. These estimates are rather consistent with our results. However, none of those studies had any information on previous falls and physical function, factors that seemed to impact the results in our analyses. Also, no BMD measurements were made. A more striking association between PAD and hip fracture risk was found in a study of more than 30,000 twins from the Swedish twin registry, reporting an increased risk of hip fracture in men and women with a hospital diagnosis of PAD with an HR of 3.20 (95% CI 2.28–4.50), independently of age and several diseases [19]. Further adjustments for lifestyle factors were described to marginally change the estimate, but no data were presented. In contrast, in a register-based study of nearly 190,000 Spanish men ≥ 65 years of age, Reyes et al. found a significantly increased risk of hip fracture in men with PAD in an age-adjusted model (RR 1.45; 95% CI 1.20–1.74), but when adding BMI, smoking status, medical use and comorbidities including other CVD, the association declined significantly (RR 1.13; 95% CI 0.87–1.48) [29]. Moreover, Collins et al. who conducted a similar study to ours but in the US cohort of MrOS, found an increased risk for non-spine fractures in men with PAD independently of hip BMD, but no association with hip fracture risk was observed [16]. The latter lack of association might, however, have been influenced by the limited number of hip fractures during follow-up (n = 89).
Finally, a few smaller studies assessing this topic found no association between PAD and fracture risk. A study of 72 residents in a nursing home confirmed increased mortality in residents with an ABI < 0.9 or ≥ 1.4, but the incidence of hip fractures ended up being too low to study as an outcome [23]. Likewise, a cohort study with 1332 men and women reported no association between PAD and fracture risk, which again could be explained by the limited sample size, but also an ABI cut-off at ≤ 0.9 instead of < 0.9 [22]. Furthermore, a longitudinal study with 3626 men and women did not find any association between ABI values and hip fracture risk [18]. However, they analyzed the ABI per unit increase in the index, which is dubious to compare with the clinically more relevant cut-off value of ABI < 0.9 [18].
In summary, several prior studies support an increased risk for hip fractures in men with PAD, but conflicting results exist. The diversity in study design, especially the inconsistent choice of covariates included in the multivariate analyses, might explain some of the differences in estimates of risk as well as limit the possibility to interpret possible mechanisms. A similar concern was raised by Ungpraset et al. in their meta-analysis from 2018, including 6 of the studies described above. The authors reported a pooled RR of 1.64 (95% CI 1.17–2.29) for incident hip fracture in patients with PAD compared to patients without PAD, but highlighted the high between-study heterogeneity and possibility of publication bias [30]. Unlike most of these prior studies, we included both comorbidity and functional measurements in our multivariate analysis, which can explain the final non-significant association between PAD and hip fracture risk, despite the relatively large sample size and fracture incidence. However, the risk for type II error should also be considered, since an even larger study sample might be needed to confirm small differences between groups. Moreover, we cannot rule out the possibility of multicollinearity or overadjustment by the inclusion of non-important factors as contributing explanations for the non-significant result in our final model.
BMD in the relationship between PAD and fractures
Only three of the above-mentioned previous studies had information on BMD. Two of those find no association between fracture risk and PAD in unadjusted analyses, and further adjustments for BMD measurements were not done [18, 22]. The findings from the third one, the study from Collins et al., did not show any significant indications that hip BMD would be of major importance in the relationship between PAD and non-spine fractures, despite the lower BMD in men with PAD at baseline [16]. Consistently, in our study, men with PAD had lower baseline total body and hip BMD than men without PAD. Although this is a cross-sectional observation not adjusted for age, it is still in line with studies reporting an association between imaging and clinical manifestations of atherosclerosis and lower BMD, mostly in women but also in men [1, 12]. Common pathophysiological pathways in the development of atherosclerosis and osteoporosis could be one explanation, as some biological factors are present in both calcification of the vascular wall and the bone formation process, not only as an effect of aging [31, 32]. In addition, reduced arterial blood flow in the hip region and lower extremities might affect bone homeostasis and cause local bone loss in individuals with PAD [33]. However, this study cannot give further answers to such hypotheses as no specific measurements of vascular calcification or local blood flow were obtained. Despite these findings and the fact that low BMD is one of the most important risk factors for fragility fractures, including BMD in our multivariate analysis did not alter the association between PAD and fracture risk in a significant way. To our knowledge, our study is the first one to identify an association between PAD and increased hip fracture independent of hip BMD.
Increased fracture risk — potential mechanisms and contributing factors
Our results suggest a low probability for the association between PAD and hip fracture risk to significantly be mediated by BMD. Hence, although individuals with PAD might suffer from poor BMD, our results suggest that the impact of impaired hip BMD might be of minor importance for the overall fracture risk in men with PAD. Although we cannot ascertain any mechanistic explanation from our observational study, a number of possible contributing factors are discussed below.
First, the hypothesis of a positive association between PAD and hip fractures might be intuitive, given the number of overlapping risk factors, such as sedentary lifestyle, smoking, renal impairment, and diabetes mellitus [13, 34,35,36]. Low-grade inflammation is another factor that has been linked to both impaired bone health and peripheral atherosclerosis [25, 37], consistent with our findings of a higher level of baseline hsCRP in men with PAD. Smoking is a major risk factor for fractures [38] and a particularly strong risk factor for PAD [39]. Concurrently, in our cohort men with PAD were almost 3 times more often current smokers than men without PAD. Cadmium exposure has been proposed to account for a substantial part of the atherosclerotic effect of smoking [40], but other sources of cadmium exposure could be contributing as well, as urine cadmium levels have been associated with increased risk for new-onset PAD independently of smoking status [41]. Accordingly, in a sub-analysis from the Gothenburg part of MrOS where urine cadmium levels were obtained, we found baseline urine cadmium to be higher among men with PAD. Increased urinary cadmium has also been associated with increased risk for low BMD and fractures, even at relatively low exposure [42]. Diabetes mellitus is another established risk factor for both PAD and fractures, including hip fractures [2, 9]. Interestingly, the increased fracture risk attributed to diabetes has not been explained by loss of BMD or bone quality, but instead yet not fully known mechanisms [43, 44]. Although the results from our different Cox regression analyses showed no clear indication that any of those factors alone explain the association between PAD and fracture risk, the sum of the influence from several of those attenuated the point estimates and precision in the multivariate analyses, indicating that these factors might be of importance for the observed relationship between PAD and fracture risk.
Secondly, baseline measurements confirmed overall more morbidity and signs of frailty in men with PAD, a burden that generally could enhance the risk of injurious falls and fractures. PAD itself might cause frailty by limiting the ability to physical activity, directly due to lower limb symptoms, and indirectly through its close relationship with ischemic heart disease and stroke [2]. Indeed, observational evidence suggests that at least stroke is an independent risk factor for hip fractures [45]. Also, PAD has independently been associated with lower physical function also among asymptomatic individuals [4, 46]. In this case, the lower physical function might serve both as a potential confounder in the relationship between PAD and fracture risk (being a cause of a long-term sedentary lifestyle contributing to the development of PAD), or a mediating factor (as a result of PAD itself). Despite whether any of those assumptions is more true than the other, when including measures of handgrip strength and walking speed in the multivariate model, the association between PAD and hip fracture weakened. Additionally, walking speed was found to be the only variable that in itself attenuated the association between PAD and hip fracture risk to a non-significant level, despite the rather small absolute difference in walking speed between men with and without PAD at baseline. This strengthens the hypothesis that physical function is of importance in the relationship between PAD and hip fracture risk.
Finally, the findings of a similar pattern for all fractures and major osteoporotic in men with PAD as for hip fractures supports the main results observed for hip fracture risk (with an increased fracture risk independent of age and hip BMD, but a non-significant association in the multivariate model). The fact that the association with vertebral fractures was more uncertain strengthens the hypothesis that the increased fracture risk in men with PAD more probably is a consequence of more injurious falls rather than just low BMD. This since the latter to a higher extent leads to more spontaneous compressions of the vertebrae whereas other fracture sites, especially at the hip, ultimately are a consequence of a fall or other trauma (although the energy often is low).
Strengths and limitations
This study has several strengths, including the population-based study design with a relatively large cohort prospectively followed for 10 years. Study participants were well characterized at baseline according to standardized assessments, including bone and muscle measurements, making it possible to adjust for established confounding factors. The Swedish public health care system enables reliable coverage of all fractures diagnosed in hospitals. Additionally, all fractures were verified by x-ray, providing a low risk of misclassification. However, our study also has limitations. Firstly, this study consisted almost entirely of elderly Caucasian men. This is a highly relevant study population, as Caucasians in general, and Swedes in particular, are particularly susceptible to hip fractures [35], but also limits the generalizability of our findings. In addition, the frailest men may have declined participation, according to inclusion criteria and the extensive baseline exams that might have contributed to such selection bias. The questionnaires relied on self-reported data, which might cause recall bias. Finally, inherent to an observational study, causal conclusions must be carefully assessed. We have adjusted for relevant confounders in our analyses; however, residual confounding cannot be ruled out.
Conclusion
The results of this study suggest that PAD is associated with an increased risk for hip fracture independently of hip BMD in elderly Swedish men. However, the high frequency of comorbidity and lower physical performance among these men are factors that together could explain much of the observed association. In a clinical setting, it could be valuable to assess the overall fracture risk in elderly men with PAD such as optimizing cardiovascular prevention, encouraging physical activity, and preventing injurious fall accidents. However, according to our results, bone density measurements should be done based on similar risk analysis as for any other older man. Future research is warranted to confirm or contradict these findings and to further address how PAD according to fracture risk best should be handled in clinical practice.
References
den Uyl D, Nurmohamed MT, van Tuyl LHD, Raterman HG, Lems WF (2011) (Sub)clinical cardiovascular disease is associated with increased bone loss and fracture risk; a systematic review of the association between cardiovascular disease and osteoporosis. Arthritis Res Ther 13(1):R5. https://doi.org/10.1186/ar3224
Aboyans V, Ricco JB, Bartelink MLEL et al (2018) 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J 39:763–816. https://doi.org/10.1093/eurheartj/ehx095
Fowkes FGR, Rudan D, Rudan I et al (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 382:1329–1340. https://doi.org/10.1016/S0140-6736(13)61249-0
McDermott MM, Greenland P, Liu K et al (2001) Leg symptoms in peripheral arterial disease associated clinical characteristics and functional impairment. JAMA 286:1599–1606
Gardner AW, Montgomery PS (2001) Impaired balance and higher prevalence of falls in subjects with intermittent claudication. J Gerontol A Biol Sci Med Sci 56:M454–M458. https://doi.org/10.1093/gerona/56.7.M454
McDermott MM, Guralnik JM, Ferrucci L et al (2008) Asymptomatic peripheral arterial disease is associated with more adverse lower extremity characteristics than intermittent claudication. Circulation 117:2484–2491. https://doi.org/10.1161/CIRCULATIONAHA.107.736108
Wong SY, Kwok T, Woo J, Lynn H, Griffith JF, Leung J, Tang YY, Leung PC (2005) Bone mineral density and the risk of peripheral arterial disease in men and women: results from Mr. and Ms Os. Hong Kong Osteoporos Int 16:1933–1938. https://doi.org/10.1007/s00198-005-1968-3
Forbes JM, Cooper ME (2013) Mechanisms of diabetic complications. Physiol Rev 93:137–188. https://doi.org/10.1152/physrev.00045.2011
Moayeri A, Mohamadpour M, Mousavi SF, Shirzadpour E, Mohamadpour S, Amraei M (2017) Fracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysis. Ther Clin Risk Manag 13:455–468. https://doi.org/10.2147/TCRM.S131945
Bentler SE, Liu L, Obrizan M et al (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170:1290–1299. https://doi.org/10.1093/aje/kwp266
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194. https://doi.org/10.1359/JBMR.050304
Ye C, Xu M, Wang S, Jiang S, Chen X, Zhou X, He R (2016) Decreased bone mineral density is an independent predictor for the development of atherosclerosis: a systematic review and meta-analysis. PLoS One 11:e0154740. https://doi.org/10.1371/journal.pone.0154740
Anagnostis P, Karagiannis A, Kakafika AI, Tziomalos K, Athyros VG, Mikhailidis DP (2009) Atherosclerosis and osteoporosis: age-dependent degenerative processes or related entities? Osteoporos Int 20:197–207. https://doi.org/10.1007/s00198-008-0648-5
Baldwin MJ, Policha A, Maldonado T, Hiramoto JS, Honig S, Conte MS, Berger J, Rockman CB (2017) Novel association between bone mineral density scores and the prevalence of peripheral artery disease in both sexes. Vasc Med 22:13–20. https://doi.org/10.1177/1358863x16672740
van der Klift M, Pols HA, Hak AE, Witteman JC, Hofman A, de Laet CE (2002) Bone mineral density and the risk of peripheral arterial disease: the Rotterdam Study. Calcif Tissue Int 70:443–449. https://doi.org/10.1007/s00223-001-2076-9
Collins TC, Ewing SK, Diem SJ, Taylor BC, Orwoll ES, Cummings SR, Strotmeyer ES, Ensrud KE (2009) Peripheral arterial disease is associated with higher rates of hip bone loss and increased fracture risk in older men. Circulation 119:2305–2312. https://doi.org/10.1161/circulationaha.108.820993
Liang DK, Bai XJ, Wu B, Han LL, Wang XN, Yang J, Chen XM (2014) Associations between bone mineral density and subclinical atherosclerosis: a cross-sectional study of a Chinese population. J Clin Endocrinol Metab 99:469–477. https://doi.org/10.1210/jc.2013-2572
Barzilay JI, Buzkova P, Cauley JA, Robbins JA, Fink HA, Mukamal KJ (2018) The associations of subclinical atherosclerotic cardiovascular disease with hip fracture risk and bone mineral density in elderly adults. Osteoporos Int 29:2219–2230. https://doi.org/10.1007/s00198-018-4611-9
Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, Pedersen NL, Michaëlsson K (2009) Cardiovascular diseases and risk of hip fracture. JAMA 302:1666–1673. https://doi.org/10.1001/jama.2009.1463
Hyde Z, Mylankal KJ, Hankey GJ, Flicker L, Norman PE (2013) Peripheral arterial disease increases the risk of subsequent hip fracture in older men: the Health in Men Study. Osteoporos Int 24:1683–1688. https://doi.org/10.1007/s00198-012-2218-0
Liu FL, Lin CS, Yeh CC, Shih CC, Cherng YG, Wu CH, Chen TL, Liao CC (2017) Risk and outcomes of fracture in peripheral arterial disease patients: two nationwide cohort studies. Osteoporos Int 28:3123–3133. https://doi.org/10.1007/s00198-017-4192-z
von Muhlen D, Allison M, Jassal SK, Barrett-Connor E (2009) Peripheral arterial disease and osteoporosis in older adults: the Rancho Bernardo Study. Osteoporos Int 20:2071–2078. https://doi.org/10.1007/s00198-009-0912-3
Peláez VC, Ausín L, Mambrilla MR, Gonzalez-Sagrado M, Castrillón JLP (2015) Ankle-brachial index, risk of clinical fractures, mortality and low bone mass in nursing home residents. Eur Rev Med Pharmacol Sci 19:1577–1582
Tivesten Å, Mellström D, Jutberger H, Fagerberg B, Lernfelt B, Orwoll E, Karlsson MK, Ljunggren Ö, Ohlsson C (2007) Low serum testosterone and high serum estradiol associate with lower extremity peripheral arterial disease in elderly men. The MrOS Study in Sweden. J Am Coll Cardiol 50:1070–1076. https://doi.org/10.1016/j.jacc.2007.04.088
Eriksson AL, Moverare-Skrtic S, Ljunggren O, Karlsson M, Mellstrom D, Ohlsson C (2014) High-sensitivity CRP is an independent risk factor for all fractures and vertebral fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 29:418–423. https://doi.org/10.1002/jbmr.2037
Austin PC, Lee DS, Fine JP (2016) Introduction to the analysis of survival data in the presence of competing risks. Circulation 133:601–609. https://doi.org/10.1161/CIRCULATIONAHA.115.017719
Schisterman EF, Cole SR, Platt RW (2009) Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20:488–495. https://doi.org/10.1097/EDE.0b013e3181a819a1
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Reyes C, Estrada P, Nogués X, Orozco P, Cooper C, Díez-Pérez A, Formiga F, MácIas JG, Prieto-Alhambra D (2014) The impact of common co-morbidities (as measured using the Charlson index) on hip fracture risk in elderly men: a population-based cohort study. Osteoporos Int 25:1751–1758. https://doi.org/10.1007/s00198-014-2682-9
Ungprasert P, Wijarnpreecha K, Thongprayoon C, Cheungpasitporn W (2018) Peripheral arterial disease and risk of hip fracture: a systematic review and meta-analysis of cohort studies. J Postgrad Med 64:220–225. https://doi.org/10.4103/jpgm.JPGM_685_17
Lampropoulos CE, Papaioannou I, D’Cruz DP (2012) Osteoporosis - a risk factor for cardiovascular disease? Nat Rev Rheumatol 8:587–598. https://doi.org/10.1038/nrrheum.2012.120
Karwowski W, Naumnik B, Szczepański M, Myśliwiec M (2012) The mechanism of vascular calcification - a systematic review. Med Sci Monit 18:RA1–RA11
Fehervari M, Sarkadi H, Krepuska M, Sotonyi P, Acsady G, Entz L, Lakatos P, Szeberin Z (2013) Bone mineral density is associated with site-specific atherosclerosis in patients with severe peripheral artery disease. Calcif Tissue Int 93:55–61. https://doi.org/10.1007/s00223-013-9727-5
Criqui MH, Aboyans V (2015) Epidemiology of peripheral artery disease. Circ Res 116:1509–1526. https://doi.org/10.1161/CIRCRESAHA.116.303849
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Goto NA, Weststrate ACG, Oosterlaan FM, Verhaar MC, Willems HC, Emmelot-Vonk MH, Hamaker ME (2020) The association between chronic kidney disease, falls, and fractures: a systematic review and meta-analysis. Osteoporos Int 31:13–29. https://doi.org/10.1007/s00198-019-05190-5
Cauley JA, Kassem AM, Lane NE, Thorson S (2016) Prevalent peripheral arterial disease and inflammatory burden. BMC Geriatr 16:213. https://doi.org/10.1186/s12877-016-0389-9
Kanis JA, Johnell O, Oden A et al (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162. https://doi.org/10.1007/s00198-004-1640-3
Banks E, Joshy G, Korda RJ, Stavreski B, Soga K, Egger S, Day C, Clarke NE, Lewington S, Lopez AD (2019) Tobacco smoking and risk of 36 cardiovascular disease subtypes: fatal and non-fatal outcomes in a large prospective Australian study. BMC Medicine 17: 128. https://doi.org/10.1186/s12916-019-1351-4
Navas-Acien A, Selvin E, Sharrett AR, Calderon-Aranda E, Silbergeld E, Guallar E (2004) Lead, cadmium, smoking, and increased risk of peripheral arterial disease. Circulation 109:3196–3201. https://doi.org/10.1161/01.CIR.0000130848.18636.B2
Tellez-Plaza M, Guallar E, Fabsitz RR, Howard BV, Umans JG, Francesconi KA, Goessler W, Devereux RB, Navas-Acien A (2013) Cadmium exposure and incident peripheral arterial disease. Circ Cardiovasc Qual Outcomes 6:626–633. https://doi.org/10.1161/CIRCOUTCOMES.112.000663
Wallin M, Barregard L, Sallsten G, Lundh T, Karlsson MK, Lorentzon M, Ohlsson C, Mellström D (2016) Low-level cadmium exposure is associated with decreased bone mineral density and increased risk of incident fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 31:732–741. https://doi.org/10.1002/jbmr.2743
Schwartz AV (2016) Epidemiology of fractures in type 2 diabetes. Bone 82:2–8. https://doi.org/10.1016/j.bone.2015.05.032
Shanbhogue VV, Hansen S, Frost M, Brixen K, Hermann AP (2017) Bone disease in diabetes: another manifestation of microvascular disease? Lancet Diabetes Endocrinol 5:827–838. https://doi.org/10.1016/S2213-8587(17)30134-1
Luan L, Li R, Wang Z, Hou X, Gu W, Wang X, Yan S, Xu D (2016) Stroke increases the risk of hip fracture: a systematic review and meta-analysis. Osteoporos Int 27:3149–3154. https://doi.org/10.1007/s00198-016-3632-5
Matsushita K, Ballew SH, Sang Y et al (2017) Ankle-brachial index and physical function in older individuals: the atherosclerosis risk in communities (ARIC) study. Atherosclerosis 257:208–215. https://doi.org/10.1016/j.atherosclerosis.2016.11.023
Acknowledgements
We thank the staff and participants of the MrOS Sweden study for their important contributions.
Funding
Open access funding provided by University of Gothenburg. This study was supported by the ALF/LUA research grant from the Sahlgrenska University Hospital.
Author information
Authors and Affiliations
Contributions
Study design and data collection for MrOS Sweden: DM, CO, ML, MK, ÖL. Study design for present work: TB, DM, and KM. Data analysis: TB and DM together with a professional statistician. Data interpretation: TB, DM, and KM. Drafting manuscript: TB. Revising manuscript content and approving the final version: All authors. TB and DM take responsibility for the integrity of the data analysis.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The ethics committees at the Universities of Gothenburg, Lund, and Uppsala approved the study. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Mattias Lorentzon has received lecture fees from Astellas, Amgen, Lilly, Meda, Renapharma, UCB Pharma, and consulting fees from Amgen, Radius Health, UCB Pharma, Renapharma and Consilient Health, all outside the submitted work. All other authors state that they have no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bokrantz, T., Manhem, K., Lorentzon, M. et al. The association between peripheral arterial disease and risk for hip fractures in elderly men is not explained by low hip bone mineral density. Results from the MrOS Sweden study. Osteoporos Int 33, 2607–2617 (2022). https://doi.org/10.1007/s00198-022-06535-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06535-3