Abstract
Background
Indications for kidney biopsy in adult IgA vasculitis (IgAV) remain debated and there are very few studies on this subject. The aim of this study was to establish a correlation between renal histological and clinical-laboratory data.
Methods
A retrospective multicenter study was conducted using three databases from French hospitals, gathered between 1977 and 2020. The study included 294 adult patients with IgAV who had undergone kidney biopsy assessed according to the prognostic “Pillebout classification”. Different statistical models were used to test the correlations between histological and clinical-laboratory data: Cochran Armitage, ANOVA, Kruskal–Wallis and logistic regression.
Results
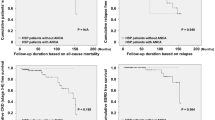
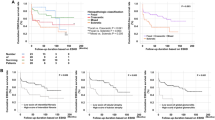
The patients were primarily men (64%), with a mean age of 52 years. The main organs and tissues involved were: dermatological 100%, digestive 48% and rheumatological 61%. All had features of kidney involvement. The median serum creatinine was 96 µmol/L serum albumin 35 g/L, and C-reactive protein 28 mg/L. Of the patients, 86% (n = 254) had hematuria and median proteinuria was 1.8 g/day. The only statistically significant correlation between the pathological stages and the clinical-laboratory data was the presence of hematuria (p = 0.03, 66% class I to 92% class IV). In multivariate analysis, only albuminemia was associated with extracapillary proliferation (p = 0.02; OR 0.94) and only age was associated with stages 3–4 (p = 0.03; OR 1.02).
Conclusion
Our study suggests that there is no strict baseline correlation between renal pathology and clinical-laboratory data. Given the current knowledge, it seems relevant to recommend a kidney biopsy in the presence of significant and persistent proteinuria or unexplained kidney function decline.
Graphical abstract



Similar content being viewed by others
Abbreviations
- CRP:
-
C-reactive protein
- CNIL:
-
« Commission Nationale de l'Informatique et des Libertés»
- eGFR:
-
Estimated glomerular filtration Rate
- ESRD:
-
End-stage renal disease
- GI:
-
Gastroenterological involvement
- HSPN:
-
Henoch–Schönlein Purpura Nephritis
- IgA:
-
Immunoglobulin A
- IgAV:
-
IgA vasculitis
- IQR:
-
Interquartile range
- MDRD:
-
Modification of diet in renal disease
- IgAN:
-
IgA nephropathy
- Q1:
-
First quartile
- Q3:
-
Third quartile
- SD:
-
Standard deviation
References
Jennette JC, Falk RJ, Bacon PA et al (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65(1):1–11. https://doi.org/10.1002/art.37715
Audemard-Verger A, Pillebout E, Guillevin L, Thervet E, Terrier B (2015) IgA vasculitis (Henoch-Shönlein purpura) in adults: diagnostic and therapeutic aspects. Autoimmun Rev 14(7):579–585. https://doi.org/10.1016/j.autrev.2015.02.003
Shrestha S, Sumingan N, Tan J et al (2006) Henoch Schönlein purpura with nephritis in adults: adverse prognostic indicators in a UK population. QJM Mon J Assoc Physicians 99(4):253–265. https://doi.org/10.1093/qjmed/hcl034
Pillebout E, Sunderkötter C (2021) IgA vasculitis. Semin Immunopathol. https://doi.org/10.1007/s00281-021-00874-9
Lu S, Liu D, Xiao J et al (2015) Comparison between adults and children with Henoch–Schönlein purpura nephritis. Pediatr Nephrol Berl Ger 30(5):791–796. https://doi.org/10.1007/s00467-014-3016-z
Coppo R, Mazzucco G, Cagnoli L, Lupo A, Schena FP (1997) Long-term prognosis of Henoch–Schönlein nephritis in adults and children. Italian Group of Renal Immunopathology Collaborative Study on Henoch–Schönlein purpura. Nephrol Dial Transplant 12(11):2277–2283. https://doi.org/10.1093/ndt/12.11.2277
Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D (2002) Henoch–Schönlein Purpura in adults: outcome and prognostic factors. J Am Soc Nephrol JASN 13(5):1271–1278. https://doi.org/10.1097/01.asn.0000013883.99976.22
Jelusic M, Sestan M, Cimaz R, Ozen S (2019) Different histological classifications for Henoch–Schönlein purpura nephritis: which one should be used? Pediatr Rheumatol Online J 17(1):10. https://doi.org/10.1186/s12969-019-0311-z
Halimi JM, Gatault P, Longuet H et al (2020) Major bleeding and risk of death after percutaneous native kidney biopsies: a French nationwide cohort study. Clin J Am Soc Nephrol CJASN 15(11):1587–1594. https://doi.org/10.2215/CJN.14721219
Audemard-Verger A, Terrier B, Dechartres A et al (2017) Characteristics and management of IgA vasculitis (Henoch–Schönlein) in adults: data from 260 patients included in a french multicenter retrospective survey. Arthritis Rheumatol Hoboken NJ 69(9):1862–1870. https://doi.org/10.1002/art.40178
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130(6):461–470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Sethi S, Fervenza FC (2019) Standardized classification and reporting of glomerulonephritis. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 34(2):193–199. https://doi.org/10.1093/ndt/gfy220
Bertani T, Mazzucco G, Monga G (2002) How glomerular extracapillary proliferation might lead to loss of renal function: light microscopic and immunohistochemical investigation. Nephron 91(1):74–78. https://doi.org/10.1159/000057607
Don BR, Kaysen G (2004) Serum albumin: relationship to inflammation and nutrition. Semin Dial 17(6):432–437. https://doi.org/10.1111/j.0894-0959.2004.17603.x
Davin JC, Coppo R (2014) Henoch–Schönlein purpura nephritis in children. Nat Rev Nephrol 10(10):563–573. https://doi.org/10.1038/nrneph.2014.126
Suzuki H, Kiryluk K, Novak J et al (2011) The pathophysiology of IgA nephropathy. J Am Soc Nephrol JASN 22(10):1795–1803. https://doi.org/10.1681/ASN.2011050464
Komatsu H, Fujimoto S, Yoshikawa N, Kitamura H, Sugiyama H, Yokoyama H (2016) Clinical manifestations of Henoch–Schönlein purpura nephritis and IgA nephropathy: comparative analysis of data from the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol 20(4):552–560. https://doi.org/10.1007/s10157-015-1177-0
Hj O, Sv A, De Y et al (2012) Clinical outcomes, when matched at presentation, do not vary between adult-onset Henöch-Schönlein purpura nephritis and IgA nephropathy. Kidney Int. https://doi.org/10.1038/ki.2012.302
Pillebout E (2021) IgA vasculitis and IgA nephropathy: same disease? J Clin Med 10(11):2310. https://doi.org/10.3390/jcm10112310
Cattran DC, Coppo R, Working Group of the International IgA Nephropathy Network and the Renal Pathology Society et al (2009) The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 76(5):534–545. https://doi.org/10.1038/ki.2009.243
Yu B, Shi S, Hou W et al (2021) Evaluation of the Oxford classification in immunoglobulin A vasculitis with nephritis: a cohort study and meta-analysis. Clin Kidney J 14(2):516–525. https://doi.org/10.1093/ckj/sfaa129
Calvo-Río V, Loricera J, Martín L et al (2013) Henoch–Schönlein purpura nephritis and IgA nephropathy: a comparative clinical study. Clin Exp Rheumatol 31(1 Suppl 75):S45-51
Ye Q, Shang SQ, Liu AM et al (2015) 24h urinary protein levels and urine protein/creatinine ratios could probably forecast the pathological classification of HSPN. PLoS ONE 10(5):e0127767. https://doi.org/10.1371/journal.pone.0127767
Lu S, Liu D, Xiao J et al (2016) Correlation between clinical and pathological characteristics of Henoch–Schönlein purpura nephritis in adults. Iran J Kidney Dis 11(1):12–17
Zhong ZX, Tan JX, Tang Y, Tan L, Pei GQ, Qin W (2019) Crescent lesions are not a predictive factor in adult-onset Henoch–Schönlein purpura nephritis. Clin Exp Med 19(4):449–456. https://doi.org/10.1007/s10238-019-00567-6
Tan J, Tang Y, Xu Y et al (2019) The clinicopathological characteristics of Henoch–Schönlein purpura nephritis with presentation of nephrotic syndrome. Kidney Blood Press Res 44(4):754–764. https://doi.org/10.1159/000501459
Acknowledgements
We warmly thank Amélie Le Gouge for her precious help in statistical management and the CHRU of Tours for its support.
Author information
Authors and Affiliations
Contributions
VM, AAV: design, data analysis and writing. JMH, CB: design and writing. EP, ET, BT, ZEO, YR, FM: writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
The content of this article confirmed to ethical guidelines of the Helsinki declaration (as revised in Tokyo 2004). Both Pillebout and IGAVAS databases had already been approved by the institutional review boards. Procedures for data collection and management of patients recruited in the nephrology department of the Tours university hospital were approved by the “Commission Nationale de l'Informatique et des Libertés” (CNIL), the independent National Ethics Committee protecting human rights in France (MR-004 registration number F20210304102053).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maisons, V., Halimi, JM., Barbet, C. et al. Towards better indications for kidney biopsy in adult IgA vasculitis: a clinical-laboratory and pathology correlation study. J Nephrol 36, 485–494 (2023). https://doi.org/10.1007/s40620-022-01389-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01389-8