Abstract
During the Coronavirus-19 pandemic, chest X-ray scoring system have been validated by Al-Smadi and Toussie in this group of patients and even RALE score, previously designed for ARDS, have been used to estimate correlation with mortality. The aim of this study was to evaluate the prognostic value of As-Smadi, Tuossie and RALE scores in predicting death in the same population of patients when associated to clinical data. In this retrospective clinical study, data of patients with COVID-19, admitted to our hospital from 1st October 2020 to 31st December 2020 were collected. CXR images of each patient were analyzed with the three different scores above mentioned. 144 patients (male 96 aged 68.5 years) were included in the study. 93 patients reported a least 1 comorbidity and 36 died. The association with increasing age, presence of comorbidities, and lower hemoglobin was significantly associated with risk of death for all the regression models. When considering the radiological score, a significant effect was found for the Al Smadi and RALE scores, while no evidence of association was found for the Toussie score. The fraction of new information is 16.7% for the Al Smadi score, 12.9% for the RALE and 5.1% for the Toussie score. The improvement in the prognostic usefulness with respect to the base model is particularly interesting for the Al Smadi score. The highest c-index was also obtained by the model with the Al Smadi score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first appearance at the end of 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has rapidly spread worldwide causing the pandemic named Coronavirus Disease 2019 (COVID-19) which affected more than 264 millions of people, leading to deaths, more than 5 million of them, until the beginning of December 2021 [1].
Several publications have supported the role of chest computed tomography (CT) in early diagnosis to predict the severity of the disease and its prognosis [2,3,4]. A number of scores have been suggested to assess the severity of the disease [5]and even artificial intelligence (AI) using deep-learning (DL) algorithms has been used to improve diagnostic accuracy, lowering false-negative rate, and aid the rapid evaluation of chest CT scans [6, 7]
However, with the progression of the pandemic the use of two-view chest radiography (CXR) as a useful and easily available screening and diagnostic tool has been recommended [8, 9].
The role of CXR in predicting the course and severity of a disease has already been highlighted during the 2002 severe acute respiratory syndrome (SARS) and the 2012 Middle Est respiratory syndrome (MERS) outbreaks [10]. Toussie et al. and Al-Smadi et al. and Borghesi et al. have separately suggested scores to assess CXR in patients admitted to emergency department (ED) for COVID-19 [11,12,13]. All these scores demonstrated their utility as prognostic indicators of poorer outcome in COVID-19 patients, although the first one has been tested only on young-middle-aged adults. Furthermore, radiographic assessment of the quantity of lung edema (RALE) score, initially proposed by Warren et al. [14] to evaluate patients affected by ARDS, have been used to estimate the degree of pulmonary involvement in this group of patients and its correlation with mortality [15, 16].
Even if the utility of CXR evaluation in patients with COVID-19 has been already demonstrated, in none of the previous studies the prognostic value of the different radiographic scoring systems has been compared. In addition, to the best of our knowledge, the prognostic value of the different CXR scores has never been analyzed using a multiple regression model which takes into consideration also demographic, hematologic, and clinical data collected at the time of hospital admission.
The aim of this study was to evaluate the prognostic value of As-Smadi, Tuossie and RALE scores in predicting death in the same population of patients admitted to our hospital for COVID-19 infection. The availability of information regarding the prognostic value of the above mentioned CXR scores might be useful in the clinical practice as well as in outcome research. The results here reported suggest that several factors might be associated with death in patients with COVID-19.
Materials and methods
In this retrospective clinical study, clinical, hematologic and demographical data of patients with COVID-19 infection who were admitted to the Pneumology Unit hospital in the period from 1st October 2020 to 31st December 2020 were analyzed. The study was approved by our local ethic committee.
Inclusion criteria were: diagnosis of COVID-19 infection (confirmed through revers transcription polymerase chain reaction, RT-PCR, for SARS-CoV2), availability of CXR images performed within 5 days from hospital admission or from RT-PCR positivity (for patients who developed the infection during hospital stay).
Clinical, hematologic and demographical data included age, sex, smoking habit, comorbidities, symptoms at presentation, laboratory results were collected as well as information regarding the treatments performed during hospitalization and the hospitalization course.
Radiological evaluation
Each of the enrolled patients underwent a CXR using a digital portable anteroposterior technique to avoid the spreading of virus in the radiology department. CXR images were analyzed by an experienced radiologist (MZ) on a de-identified Picture Archiving and Communication System (PACS). MZ was blinded to clinical data, except for COVID-19 positivity. Each CRX was evaluated using three different scoring systems.
-
Toussie score [11]: each lung was divided in three zones: the lower one (from the costophrenic sulcus to inferior hilar markings), the middle zone (from the inferior hilar markings to superior hilar markings) and the upper zone (from superior hilar markings to the apices). Each zone was scored 1 if opacities were detected or 0 in case of absence of abnormalities, then a total value was obtained summarizing all the scores.
-
Al-Smadi score [12]: each lung was divided into three zones (the upper zone extends from the apex to the lower border of the anterior second rib, the middle one from the lower border of anterior 2nd rib to lower border of anterior 4th rib, and the lower one from the lower border of anterior 4th rib to the lung base). According to the number of involved zones a score from 0 to 6 is assigned and the CXR is classified as COVID-19 pneumonia 1 (CoV-P1 if the total score is < 4) or COVID-19 pneumonia 2 (CoV-P2 if the total score is ≥ 4).
-
RALE score [14]: radiograph was divided into quadrants, defined vertically by the vertebral column and horizontally by the first branch of the left main bronchus. Each quadrant was assigned a consolidation (0–4) and a density score (1–3). The final RALE score is sum of the products of the consolidation and density score for each quadrant and ranges from 0 (no infiltrates) to 48 (dense consolidation in > 75% of each quadrant).
Statistical analysis
Data were presented as mean ± standard deviation (SD) for continuous variables or frequency and percentage for categorical variables. Continuous variables were compared using the t test while categorical variables were compared using the Chi-Square since a normal distribution was found at Kolmogorov–Smirnov test. The association between clinical and demographic characteristics and death as outcome was also evaluated using logistic regression analysis. According to these results and to the percentage of missing data for each variable, a multiple logistic regression model was established (base model). The rule of thumb of considering about 10 events for each included variable was considered in building the multivariable model. Continuous variables were modelled using restricted cubic splines with 3 knots to account for possible mild non-linearities. Comorbidities significantly associated with death were grouped together in one single variable highlighting the presence of at least one of these comorbidities. The base model was compared with the same model with the addition of one of the radiographic scores to evaluate their prognostic added value. The explained variation of the base model (B) and of the model with the addition of a radiographic score (A) were calculated according to the variance of the predicted risks. Then the fraction of new information provided by the score was calculated as 1-B/A [17, 18]. Calibration, i.e. how much the predicted probabilities fit the observed data, of the regression models were evaluated using a calibration plot reporting actual vs model predicted probabilities. Apparent and bias-corrected (using 500 bootstrap replicates to avoid over-optimism) estimates were reported. The discrimination ability of the models was quantified using Harrell c-index (bootstrap correct for optimism). All statistical tests were performed using the R software [19, 20] and the rms library.
Results
A total of 144 patients with a confirmed diagnosis of SARS-CoV2 infection were enrolled in this study. The majority of them were males (96 males, 48 females) with a mean age of 68.5 years (23–94). Males were significantly younger than females (66.6 ± 13.4 years and 72.3 ± 14 respectively; p = 0.02). Eight-point-five percent of the cohort was composed by patients who were referred to the Pulmonary Unit because found positive at COVID-19 infection during hospital stay for other causes. The remaining patients were referred to our unit directly from the ED of our hospital. A total of 36 patients (25%) died during hospitalization.
The more common reported comorbidities were: hypertension (45.1%), cardiovascular diseases (32.6%), diabetes mellitus (20.1%), dyslipidemia (10.4%), asthma and/or chronic obstructive pulmonary disease (9%) and obesity (8.3%). Ninety-three patients (67%) reported at least one comorbidity. The results of the comparison of the distribution of these comorbidities between patients who died and who survived are reported in Table 1. A significant difference in the prevalence of cardiovascular disease, hypertension, obesity, and pulmonary interstitial disease between patients who died and who survived was found.
As far as the symptoms are concerned, at the time of admission, fever (77.1%), dyspnea (61.8%) and cough (31.9%) were the more frequent complaints, less frequently patients complained of fatigue (11.8%), diarrhea (9%), ageusia and/or anosmia (2.1%) and myalgia (1.4%). The distribution of death according to the presence of symptoms is reported in Table 2. No significant differences were found in the distribution of death according to the presence/absence of these symptoms. Laboratory results are reported in Table 3. Significant differences were found in the distribution of procalcitonin (PCT), and D-DIMER and hemoglobin between patients according to death.
Ninety-two patients (74.2% of cases) received medical treatment with steroids, more precisely 37 received dexamethasone according the RECOVERY trial [21]and 55 methylprednisolone, following the Salton F. protocol [22]. Antibiotic and low molecular weight heparin was prescribed for 91.3% and 62.9%, respectively. No significative difference on mortality was observed between patients treated with steroid, regardless which steroids protocol was used, and the remaining dosage of the main treatment has been described in Table 4.
During the study period, patients underwent different treatments according to the clinical trial or emerging clinical recommendations, thus 11 patients received tocilizumab, 45 were put on anti-retroviral treatment (remdesivir or lopinavir/ritonavir) and hydroxychloroquine was given to 32 patients. Mean hospital stay was 19.7 ± 11.7 days. Respiratory failure was observed in all patients at the time of admission and the majority of them (56%) required positive pressure support (CPAP-Helmet), while 24% of patients required orotracheal intubation due to respiratory gas exchange deterioration during hospital stay.
Radiological evaluation
In the majority of cases, CXR showed a bilateral involvement (54.9%). The presence of ground glass opacities, consolidation and reticular interstitial pattern were observed in 43.7%, 33% and 7% respectively. In 16.3% of cases no significative abnormality was diagnosed at the CXR. In addiction no complication such as pneumothorax, pneumomediastinum, and pleural effusion was observed at the time of diagnosis.
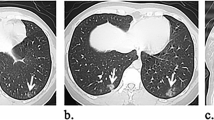
The CXR of all the patients were evaluated using the three different radiological scores (Fig. 1). According to Al-Smadi scoring system, 71 patients (49.3%) were categorized as CoV-P1, while 73 (50.7%) were categorized as CoV-P2. Death was significantly more frequent in those categorized as CoV-P2 (27 out of 73 vs 9 out of 71, p < 0.001 at Chi Square test). The mean RALE score was 11.8 ± 9.07 (0–40). The t test showed a significant difference between the RALE score obtained in patients who died and in those who survived (17.19 ± 10.51 vs 10.01 ± 7.79, p < 0.001 at t test). Finally, 15 out of 144 patients (10.4%) scored 0 at Toussie, 12 (8.3%) scored 1, 25 (17.4%) scored 2, 12 (8.3) scored 3, 37 (25.7%) scored 4, 21 (14.6%) scored 5, and 22 (15.3%) scored 6. A significant association with death was found at t test (p < 0.001). In particular, death was more frequent in patients who scored higher than 2 at Toussie score.
A 70-year-old female admitted to our hospital. Hypertension was the only co-morbidities referred. Chest radiograph at the time of admission in the hospital has been scored with Al Smadi score (A) [9], Toussie (B) [8] and RALE score (C) [10]. The radiologist observed GGO involving bilateral lower zones and right middle zone and assigned CoV-P1 category (3 points), according to the Al Smadi score and point 3 according Toussie score. The evaluation of the CXR using RALE score gave a total of 7 points as quadrant (a) was scored 1 for consolidation and 2 for density, quadrant b zero points for both the variables, quadrant (c) 2 points and (d) 1 points, both for density and consolidation
Regression analysis
Binary logistic regression was performed to assess the association among the collected variables and the event of death. The results are reported in Table 4. When considering continuous variables, a significant non-linear effect was demonstrated for age (p = 0.004) and PCT (p = 0.003). At univariate analysis, presence of comorbidities, age, reactive protein C (RPC), PCT and Hemoglobin showed a significant effect. RPC was not included in the multivariable regression model as there was no evidence of association with death according to t test (Table 3), while PCT was excluded for the number of missing measurements. At the end, a multiple logistic regression model with presence of comorbidities, age (linear and non-linear effect) and hemoglobin was estimated (Base model).Three models were then compared to the base model: model 1 was specified with the addition of the Al Smadi score; model 2 with the RALE score; model 3 with Toussie score. RALE and Toussie scores were modelled as a linear function.
As shown in Table 5, the association with age, presence of comorbidities and hemoglobin was significant for all the regression models. As expected, increasing age is associated with an increase of the risk of death. The increase in hemoglobin levels is associated with a decrease in the risk of death. The presence of comorbidities has a very strong association with the risk of death. When considering the radiological score, a significant effect was found for the Al Smadi and RALE scores, while no evidence of association was found for the Toussie score.
In Fig. 2, the calibration of the different models is reported. The calibration plots of the regression models with the addition of the chest radiography scores show improvements with respect to the baseline model, especially for the Al Smadi score. In particular, the amount of explained variation by the base model was 34.2%, while the relative explained variation and fraction of new information added by each chest radiography score are reported in Table 4. The fraction of new information is 16.7% for the Al Smadi score, 12.9% for the RALE and 5.1% for the Toussie score. The improvement in the prognostic usefulness with respect to the base model is particularly interesting for the Al Smadi score. The highest c-index was also obtained by the model with the Al Smadi score.
Calibration curves of the estimated probabilities from the different multiple regression models. Predicted vs observed values are shown by the dotted lines and called “Apparent”, i.e. without correction for optimism. Bootstrap corrected estimates (Bias-corrected) of predicted vs. observed values are shown by the solid line. Ideal calibration (dashed) corresponds to a perfectly calibrated model where actual probabilities equal predicted probability. The model with the best calibration is the one including Al Smadi score
Discussion
The outbreak of SARS-CoV2 pandemic has arisen the need of improving simple and robust predictive model, combining clinical and radiological information, to help clinicians, especially in the ED, to detect more severe patients as well as predict outcomes.
In this study a model combining age, the presence of at least one comorbidity and hemoglobin values may predict the death in adult affected by COVID-19. Interestingly, the addiction of Al-Smadi and RALE score improved the predictive power of this model as a significative effect has been observed. In the case of Toussie score, although among our population death was more frequent in patients who scored > 2 as previously observed [11], the addiction of this information to the basal model does not add significative information.
Furthermore, in our study, the improvement of prognostic power to the basal model was higher with Al-Smadi score with respect to the RALE score (16.7% vs 12.9%, respectively).
Baratella et al. [23] retrospectively evaluated 140 CXR of patients admitted to the ED in three different hospitals. CXRs were scored 0, if no lung involvement was observed, while scores1 to 4 showed the first (less severe) to the fourth (more severe) quartiles regarding the severity of lung involvement. In this study, this score was useful to predict the clinical progression in cases with no radiological involvement (0 score) or severe involvement at the CXR (scores 3–4), on the contrary in patients with a mild to moderate pattern (score 1 and 2) it was not able to give these information. Compared to our study, the characteristics of the population is similar in terms of mean age, comorbidities and symptoms at the time of presentation. Although the proportion of CXR with no lung involvement was higher in our study (5% vs 16.3%), in our case the use of invasive ventilation was required in 56% of patients compared to 38%. No major differences have been observed in terms of intubation (our study 24% vs Baratella’s 28%) and death (25% our study vs Baratella’s 20.9%).
A wide range of age is included in our study and our data confirm advanced age as a risk factor for poor prognosis in COVID-19. This observation is in line with what observed in other studies [24,25,26,27,28], and even in SARS and MERS outbreaks [29, 30]. Furthermore, the increased risk of mortality in older patients in our cohort can be due, especially at the beginning of the pandemic, to the limited availability of intensive care setting.
At least one comorbidity has been observed in the majority of patients. Cardiovascular disease, hypertension and diabetes mellitus were the most frequent and the first two were significantly more reported among dead, in line with the literature [24,25,26,27,28]. In our cohort of patients, although obesity was present in a small group of patients (8.6%), the majority of them died. Our data confirm how the presence of comorbidity, particularly cardiovascular disease, hypertension and obesity increased the risk of mortality in COVID-19 patients.
In our population PCT and D-dimer values, but not CRP were significantly higher in patients who died compared to the others. These information suggest how the presence of a bacterial co-infection and the possible presence of a vascular thromboembolism at the time of SARS-CoV-2 infection diagnosis may increase the risk of mortality.
As far as the hemoglobin level is concerned, regression analysis demonstrated a significant effect on death. This observation is in line with previous studies, in fact anemia at admission has been associated with bad prognosis in COVID-19 patients [29,30,31]. Tremblay et al. described a large cohort of patients diagnosed with COVID-19 with a vary range of clinical presentation and showed that anemia was a significant independent predictor of mortality, independently form age, gender and comorbidities. According to the authors, the value highly predictive of a bad outcome was 11.5 g/dL in men and 11.8 g/dL in women [32] and a similar value was observed in a non-survivor group by Rossio et al. [33].
In our cohort PCT values demonstrated a significative effect in the prediction of death. This test is not routinely performed in our ED, thus it was not available for all patients at the time of SARS-Cov2 diagnosis and for this reason it was not included in the regression model. However, this data suggests how bacterial superinfection may play a role in worsening the severity of the disease in these patients. This finding is in line with other studies reporting that elevated PCT values are related to the severity of COVID-19 [23,24,25, 33] In addiction a meta-analysis highlighted how increased PCT level is associated to an increase of developing severe COVID-19 (five times higher) [34]. Moreover, it was demonstrated that as the PCT increases, the disease gets worse, suggesting its utility in the prognosis of affected patients [35].
Study limitations
Even if the integration of clinical data and radiological chest imaging evaluated with three different scores in a cohort managed in the same pneumology unit represents a potential strength, there are still some important limitations in the present study. In particular, the retrospective design of the study, the small number of patients and the presence of a single rater for radiological evaluations are the most important ones. In addition, because of the high number of missing measurements for PCT, this variable was not included in the base-model even if a significant effect on death was demonstrated both at univariate analysis and with the t test. Furthermore, P/F values were not available for several patients as well as the blood gas analysis was not performed routinely in the ED and this data has been excluded from the analysis. However, it must be noted that the low number of enrolled patients is related to the fact that this study is based on the data gathered from a single center. In addition, the radiologist who performed the evaluations had more than 40 years of expertise in evaluating CXR. Nonetheless, the results here reported should be considered with caution and further studies are needed to confirm these preliminary data.
Conclusions
The results here reported suggest that several factors might be associated with death in patients with COVID-19. In particular, the explained variation of the outcome “death” reaches the value of 34% using a regression model which comprises age, presence of comorbidities, and hemoglobin measurements (34% of explained variation). By adding the results of the CXR assessment performed with the Al-Smadi and RALE scoring systems, the explained variation of this model increases. However, the fraction of new information added to the regression model is higher with the Al-Smadi scoring system than with the RALE one.
References
WHO (2021) Covid-10 weekly Epidemiological update Edition 69, published 7 2021 December.
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L (2020) Correlation of chest CT and RT-PCR Testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 296(2):E32–E40
Xie XZ, Zhong Z, Zhao W et al (2020) Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 296(2):E41–E45
Bernheim A, Mei X, Huang M et al (2020) Chest CT findings in coronavirus disease-19: relationship to duration of infection. Radiology 295(3):685–691
Prokop M, van Everdingen W, van Rees Vellinga T, van Quarles Ufford H, Stöger L, Beenen L et al (2020) CO-RADS: a categorical CT assessment scheme for patients suspected of having COVID-19-definition and evaluation. Radiology 296:97–104
Wang S, Kang B, Ma J et al (2021) A deep learning algorithm using CT images to screen for corona virus disease (COVID-19). Eur Radiol 31(8):6096–6104
Zhang K, Liu X, Shen J, Li Z, Sang Y, Wu X et al (2020) Clinically applicable AI system for accurate diagnosis, quantitative measurements, and prognosis of COVID-19 pneumonia using computed tomography. Cell 181:1423–1433
ACR (2020) Recommendations for the use of chest radiography and computer tomography for suspected COVID-19 infections. American College of Radiology, Reston
Sverzellati N, Ryerson CJ, Milanese G et al (2021) Chest x-ray or CT for COVID-19 pneumonia? Comparative study in a simulated triage setting. Eur Respir J 58(3):2004188
Hosseiny M, Kooraki S, Gholamrezanezhad A et al (2020) Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and middle east respiratory syndrome. AJR Am J Roentgenol 214(5):1078–1082
Toussie D, Voutsinas N, Finkelstein M et al (2020) Clinical and chest radiography features determine patient outcomes in young and middle-aged adults. Radiology 297:197–206
Al Smadi A, Bhatnagar A, Ali R et al (2021) Correlation of chest radiography findings with the severity and progression of covid-19 pneumonia. Clin Imaging 71:17–23
Maroldi R, Rondi P, Agazzi GM et al (2021) Which role for chest x-ray score in predicting the outcome in COVID-19 pneumonia? Europ Radiol 31:4016–4022
Warren MA, Zhao Z, Koyama T et al (2018) Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax 73(9):840–846
Au-Yoing I, Higashi Y, Giannotti E et al (2022) Chest radiograph scoring alone or combined with other risk scores for predictin outcomes in covid-19. Radiology 301(3): E444 (Online ahead of print)
Sathi S, Tiwari R, Verma R et al (2021) Role of Chest X-ray in coronavirus disease and correlation of radiological features with clinical outcomes in Indian patients. Can J infect Dis Med Microbiol. 2021:6326947 (Published online)
Schemper M (2003) Predictive accuracy and explained variation. Stat Med 22:2299–2308
Harrell FE (2015) Regression modeling strategies, with applications to linear models, logistic and ordinal regression, and survival analysis, 2nd edn. Springer, New York
R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
Frank E Harrell Jr (2021). rms: regression modeling strategies. R package version 6.2–0. https://CRAN.R-project.org/package=rms
Salton F, Confalonieri P, Meduri GU et al (2020) Prolonged low-dose methylprednisolone in patients with severe COVID-19 Pneumonia. Open Forum Infect Dis 7(10):ofaa421
The RECOVERY Collaborative Group (2021) dexamethasone in hospitalized patients with COVID-19. N Engl J Med 384:693–704
Baratella E, Crivelli P, Marrocchio C et al (2020) Severity of lung involvement on chest X-rays in SARS-Coronavirus-2 infected patients as a possible tool to predict clinical progression: an observational retrospective analysis of the relationship between radiologica, clincial and laboratory data. J Bras Pneumol 46(5):e20200226
Guan W, Ni Z, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720
Wu Z, McGoogan JM (2020) Characteristic and important lessons from the coronavirus disease 19 outbreak in China. JAMA 323(13):1239–1242
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The Lancet 395(10223):497–506
Corradini E, Ventura P, Ageno W et al (2021) Clinical factors associated with death in 3044 Covid-19 patients manged in internal medicine wards in Italy: results from the SIMI-COVID19 study of the Italian society of internal medicine (SIMI). Intern Emerg Med 16(4):1005–1015
Bandera A, Nobili A, Tettamanti M et al (2021) CLincial factors associated with death in 3044 COVID-19 patients managed in internal medicine wards in Italy: comment. Intern Emerg Med 18:1–4
Chan JW, NG CK, Chan CK, et al (2003) Short term outcome and risk factors for clinical outcomes in adults with severe acute respiratory syndrome (SARS). Thorax 58(8):686–689
Arabi YM, Balkhy HH, Hayden FG et al (2017) Middle east respiratory syndrome. N Engl J Med 376(6):584–594
Bellmann-Weiler R, Lanser L, Barket R et al (2020) Prevalence and predictive value of anemia and dysregulated iron homeostasis in patients with COVID-19 infection. J Clin Med 9:2429
Tremblay D, Rapp JL, Alpert N et al (2021) Mild anemia as a single independent predictor of mortality in patients with COVID-19. EJHaem. 2(3):319–326 (Online ahead of print)
Rossio R, Tettamanti M, Nobili A et al (2021) Clinical Risk scores for the early prediction of severe outcomes in patients hospitalized for COVID-19: comment. Intern Emerg Med 17(1):303–306 (Online ahead of print)
Lippi G, Plebani M (2020) Procalcitonin in patients with severe coronavirus disease 2019: a meta-analysis. Clin Chim Acta 505:190–191
Hu R, Han C, Pei S et al (2020) Procalcitonin levels in COVID-19 patients. Int J Antimicrob Agents 56(2):106051
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection were performed by MZ, IG and LC. DE, FM and FA: conducted the statistical analysis. The first draft of the manuscript was written by DE, AC and SH. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Human and animal rights statement
This retrospective research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki (revised version 2000) and approved by the San Giuseppe Hospital Institutional Review Board (Comitato Etico IRCCS Multimedica, approval number CE-39.2020).
Informed consent
Written informed consent was obtained from all study participants or their legal representatives.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elia, D., Mozzanica, F., Caminati, A. et al. Prognostic value of radiological index and clinical data in patients with COVID-19 infection. Intern Emerg Med 17, 1679–1687 (2022). https://doi.org/10.1007/s11739-022-02985-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-02985-z