Abstract
Purpose
Since the beginning of COVID-19 pandemic, social distancing and home confinement had a significant impact on children, especially on those with eating disorders (ED). The primary objective of this retrospective study was to describe and analyze the demographic and clinical profiles of children presenting with ED during the COVID-19 pandemic.
Methods
We conducted a retrospective review of clinical charts of patients with ED younger than 18 years who accessed the emergency department of the Bambino Gesù Children’s Hospital, Rome, between March 2019 and March 2021. Of these, we reported and compared the demographic, clinical and laboratory data before and after the COVID-19 pandemic and looked for predictors of ED severity.
Results
A total of 211 admissions for ED were recorded. The patients, mostly females (86.3%) were on average 14.1 years old. The mean weight loss on admission was 11 kg. Bradycardia was observed in 31.3% of the study sample. 16.6% of patients had an associated psychiatric disorder and 60.2% required psychotropic drugs. 68.7% of the patients required hospitalization. Respectively, 96 and 115 patients were admitted before and during the COVID-19 pandemic. The latter were hospitalized more (78.3 vs 57.3%; p = 0.001), yet for less time (19 vs 26 days; p = 0.004), had a higher mean serum creatinine (0.68 vs 0.47; p < 0.001) and were more frequently diagnosed with an associated psychiatric disorder (23.5 vs 8.3%; p = 0.003).
Conclusion
Our study shows a significant increase of hospitalizations of children with ED during the COVID-19 pandemic, along with a shorter length of stay, more psychiatric comorbidities, and some distinctive features at the laboratory work-up, such as an increase of serum creatinine and/or a reduction of serum albumin.
Level of evidence
III, evidence obtained from well-designed cohort or case–control analytic studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the onset of the COVID-19 pandemic, the introduction of never-before-experienced restrictions, such as social distancing and home confinement, has had a significant impact on children’s emotional and social spheres. Preliminary studies have shown that in the COVID-19 era, there was a general increase in negative feelings in the general population, such as fear, anxiety, and sadness [1,2,3,4,5,6,7,8,9,10]. In addition, COVID-19-related isolation has resulted in an increase in mental health conditions, such as post-traumatic stress disorder [6, 11], anxiety and depression [12, 13].
The social impact of confinement and isolation associated with lockdown has also recently been described in the pediatric field. According to an estimate by the Italian Ministry of Education, University, and Research (MIUR), approximately 8.5 million students remained at home during the pandemic [14]. The combination of these stressors could both exacerbate pre-existing mental health problems and cause their onset, in children and adolescents [15].
During such a sensitive time, individuals with psychiatric conditions are considered particularly vulnerable as their pre-existing conditions may be exacerbated by the effects of isolation and restrictions [1,2,3]. Social restrictions and the need for continuity of psychiatric treatment are thought to be linked to worsening symptoms in this group of patients [16, 17].
From these premises, patients with eating disorders (ED) may represent a population vulnerable to the effects of the COVID-19 pandemic [18, 19]. Interactions between genetic and environmental factors have been considered as crucial for ED pathogenesis, although the underlying mechanisms are still not completely recognized [20, 21]
In the most recent classification [21], ED includes the following conditions: Anorexia Nervosa (AN), characterized by excessive restriction of oral intakes associated with excessive physical activity (restrictive subtype), and periodic "binges" followed by vomiting or assumption of laxatives (binge-elimination behavior subtype); Bulimia Nervosa (BN), characterized by ingestion of large quantities of food in a short period of time (“binges”), followed by compensatory vomiting, assumption of laxatives, fasting or exercise; Non-specific ED, i.e., conditions in which the patient shows only some of the previous characteristics (avoidant/restrictive eating disorder and binge eating disorder (DAI) characterized by binges, not always followed by compensatory behaviors). Non-specific EDs can evolve into full-blown EDs. [21,22,23,24]
Currently, much has been written about the pediatric ED “epidemic” at the time of COVID-19 [25], but most articles have focused on the epidemiologic and seasonal pattern of ED in children [26], with little or no exploration of the risk factors that lead to increased severity of this condition in children.
We conducted a study on a large pediatric cohort, with the objective of describing and analyzing the clinical profiles of children presenting with ED during the COVID-19-related lockdown, to identify epidemiological and clinical predictors of ED severity before and after the COVID-19 pandemic.
Methods
We retrospectively reviewed the clinical charts of all patients with ED diagnoses younger than 18 years who accessed the Emergency Department of the Bambino Gesù Children's Hospital, IRCCS, Rome, between March 2019 and March 2021. ED diagnoses were defined according to DSM-5 criteria [24, 27]. During the study period, an internal protocol for the admission of ED patients was used, which was validated and in use prior to the start of the present research. In detail, the admission criteria used were as follows: BMI < 14, weight loss/week > 0.5 kg, systolic blood pressure < 90 mmHg, diastolic blood pressure < 70 mmHg, orthostatic hypotension, heart rate < 50 bpm, QTc > 450 ms, presence of arrhythmia, body temperature < 35 °C, electrolyte changes (potassium < 3.5 mmol/L, sodium < 135 mmol/L, phosphorus 0.5–0.8 mmol/L). Patients were identified through keyword searches in the hospital's electronic databases. Medical records were selected by searching for the key words “eating disorders”, “anorexia nervosa”. Then, cases with such discharge diagnosis, made by a child neuropsychiatrist, were manually selected through a retrospective review of their medical records.
We reported the following demographic, clinical and laboratory data: age; gender; geographic provenance, number and length of hospitalizations; staturo-ponderal data, including BMI on admission and at discharge (both values and centiles); number of relapses; previous menarche; duration of amenorrhea; diagnosis of any previous psychiatric disorder; vital signs; blood gas analysis and laboratory work-up on admission; administration of intravenous fluids; enteral nutrition; drug therapy; necessity of guarding by specialized staff. All data were gathered and stored in an electronic database.
Patients were divided into two subgroups and compared according to the access date, setting March 8, 2020 as the start of the COVID-19-related lockdown in Italy. In particular, ED diagnoses from March 9, 2019 to March 8, 2020 (pre-COVID-19 era) and from March 9, 2020 to March 8, 2021 (COVID-19 era) were considered. For patients admitted more than once, we reported and analyzed the first admission to the emergency department only. However, any access of these patients within the period of the study was defined as “relapse” and reported. Finally, we performed a binary logistic regression adopting the cutoff of admission before or after the COVID-19 outbreak as the dependent variable and all variables significant and/or interesting from the univariate analysis as the independent variables to identify potential factors reflecting ED severity.
The software IBM SPSS version 23.0 was used for statistical analysis. Continuous normally distributed variables were expressed as means and standard deviations and analyzed with the Student’s t test. Continuous non-normally distributed variables were expressed as medians and ranges and analyzed with the Mann–Whitney U test. Categorical variables were expressed as proportions and percentages and analyzed with the Chi-squared test or Fisher’s exact test (when appropriate). A p value less than 0.05 was considered statistically significant.
Ethical approval was granted by the Research Ethics Board at the Bambino Gesù Children's Hospital, IRCCS, Rome, Italy.
Results
The characteristics of the study sample are outlined in Table 1. A total of 211 ED-related admissions were recorded during the study period. Patients included were on average 14.1 (± 2.5) years old (range 5.3–17.9), mostly females (86.3%). 81% of patients came from the Lazio region. 68.7% of the patients were hospitalized, for a mean period of 22 (± 14) days. The mean weight loss on admission was 11 (± 8) kg, with a corresponding mean BMI of 15.8 (± 2.5) and median BMI percentile of 3.3 (range 0.2–14.5). About 8.5% of the patients relapsed during the study period. Bradycardia was observed in 31.3% of the study sample. Notably, 16.6% of patients were diagnosed with a psychiatric disorder other than ED, but 60.2% of the study sample required administration of psychotropic drugs, mostly aripiprazole (51.2%) and sertraline (25.6%). Most patients required intravenous fluids during hospitalization (63%), with a minority requiring enteral nutrition (23.2%, 14.2% of which continuous) due to severe cachexia.
The comparison of the clinical characteristics of the study sample before and during the COVID-19 pandemic is outlined in Table 2.
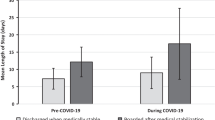
Figure 1 shows the trend in pediatric admissions by ED over the two periods. Of all patients, 96 and 115 were admitted before and during the COVID-19 pandemic, respectively. More patients required hospitalization during the COVID-19 era than before (78.3 vs 57.3%; p = 0.001), although they were significantly hospitalized for less time (19 ± 12 vs 26 ± 17 days; p = 0.004). However, no significant differences in terms of weight loss or BMI were observed between the two groups. Although not significant, a longer median time of amenorrhea was described in those who complained of it during the COVID-19 pandemic (6.2 vs 4.6 months; p = 0.100). When comparing the vital signs between the two groups, a statistically significant lower respiratory rate was detected in the COVID-19 cohort (19 ± 3 vs 16 ± 3; p < 0.001). No statistical significance was documented in terms of heart rate, bradycardia and other vital signs reported. Interestingly, the post-COVID-19 group had a higher mean serum creatinine (0.68 ± 0.26 vs 0.47 ± 0.37 mg/dl; p < 0.001) and a lower mean serum albumin (4.7 ± 0.4 vs 4.9 ± 0.4 g/dl; p = 0.001) than the patients with ED admitted before the COVID-19 pandemic. A significantly higher number of patients were diagnosed with a psychiatric disorder other than ED during the COVID-19 pandemic (23.5 vs 8.3%; p = 0.003), consequently more often requiring pharmacological treatment (71.3 vs 46.9%; p = 0.048). Aripiprazole (57.4%), sertraline (30.4%) and fluoxetine (9.6%) were the most commonly prescribed drugs in this subgroup. Moreover, patients admitted during the COVID-19 pandemic more often required intravenous fluids (72.2 vs 52.1%; p = 0.004).
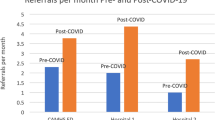
The multivariate analysis conducted on the significant variables from the univariate analysis and adjusted for age and gender proved that a shorter hospitalization, the diagnosis of a psychiatric disorder and an increased value of serum creatinine were significantly associated with admission for ED during the COVID-19 pandemic (Table 3). Figure 2 shows ED epidemiological trends during the study period.
Discussion
Our findings show a more acute and severe ED onset than in the recent past. Notably, a higher proportion of hospitalization was recorded during the COVID-19 era. Spettigue et al. also reported a higher percentage of patients requiring hospitalization during the COVID-19 pandemic: 84.2% compared to a previous 62.1% [28]. A higher rate of psychiatric disorder comorbidities and use of psychotropic drugs were detected in the COVID-19 cohort, reflecting a more complex illness. Nonetheless, the length of hospitalization was shorter during the COVID-19 pandemic rather than before. This may be due both to a more aggressive inpatient treatment of the underlying psychiatric condition as well as to the development of a solid and multi-disciplinary outpatient management of these patients, prompted by the sanitarian emergency as shown in recent reports [29]. Interestingly, patients with ED onset during the COVID-19 pandemic showed a significantly lower respiratory rate compared to the previous period. A slower respiratory rate could indicate greater severity and represent impending respiratory failure from diaphragmatic weakness. Although dehydration and electrolyte disorders are often detected in ED patients [21], blood gas analysis did not yield significant results when comparing the two subgroups. Conversely, we found a significantly higher serum creatinine and lower serum albumin in the latter group, compatible with a hyper-catabolic metabolism typical of ED patients with rapid weight loss. However, a lower serum albumin may also indicate better hydration rather than poor nutritional status. Nonetheless, more fluid was needed in the COVID-19 cohort to correct the greater dehydration in these subjects but not the rate of administration.
No significant differences to the previous year were noted in terms of weight or BMI at admission and duration of weight or BMI loss in patients admitted during the COVID-19 pandemic, suggesting to consider different parameters to evaluate ED onset severity. This is congruous to recent studies suggesting clinicians to consider different parameters to define AN severity avoiding BMI values alone [30].
On the other hand, the multivariate analysis showed that a shorter hospitalization, a psychiatric comorbidity and an increased serum creatinine were significantly associated with admission for ED during the COVID-19 pandemic, even when adjusting for BMI and weight on admission, age and gender, thus confirming the association with these factors.
Our study confirms the onset of an “epidemic within the pandemic” [31], characterized by an increased severity of ED during the COVID-19 era, which is congruous with other reports [25, 26]. As depicted in Fig. 2, the epidemiological trend of ED admissions during the COVID-19 pandemic shows an overall increase compared to the previous pre-COVID-19 year, with peaks and troughs of incidence that may be linked to emergency measures adopted by the Italian government, such as school closures (the first of which was announced on February 23, 2020) and their consequences: distance learning, home confinement, lifestyle changes [32]. Another putative cause of this increase is the temporary discontinuation of local public and private health services, which in turn can be blamed for the progression of the disease and the admission of more severely compromised patients.
Strengths and limitations
Our study has three main limitations. First, the retrospective design prevented the identification of risk factors for ED onset during the COVID-19 pandemic. Second, we could not exclude that some patients admitted during the COVID-19 era developed the disease long before this period, as in some cases, the onset of the disease can be traced back up to 6 months before the hospital admission. However, our study shows that the COVID-19 pandemic may have played a role in exacerbating the disease to the point of requiring hospital admission, rather than outpatient management. Third, some significant as well as some non-significant results may have been caused by the small sample size, rather than from an actual size effect. However, even if further multi-center research is required to clearly highlight how COVID-19 triggers and affects pediatric ED, we believe our paper provides some innovative information to add to the literature on ED onset in children.
Conclusion
Congruently with the literature, COVID-19 has been associated with worsening of mental health and development of psychiatric disorders. This study described a significant increase of ED patients during the COVID-19 pandemic among children. In particular, the presence of a psychiatric comorbidity, as well as an increase of serum creatinine and/or reduction of albumin level, should be considered as potential severity indices of ED. Families and pediatricians should be aware of the mental risk connected with the pandemic and be able to monitor and promptly detect any signs or symptoms of ED. To this regard, the development of structures where social and educational sharing can occur even in times of pandemics, may be crucial to address the complex psychological needs of teenagers. Nonetheless, more multi-center studies are required to evaluate these factors and long-term consequences of the pandemic and its related restrictions on children’s health.
What is already known on this subject?
There have been reports describing the influence of COVID-19 pandemic on eating disorders with an increase of patients affected in the pediatric age.
What this study adds?
This study highlights the increase of eating disorders during COVID-19 pandemic. It is of actual interest for readers, in the field of pediatrics eating disorders and in emergency settings, especially when the patients are conducted in the emergency department. We think that our results could be of great usefulness also for a broader audience of pediatricians and other specialists involved in children’s care.
Data availability
The datasets are available from the corresponding author on reasonable request.
Code availability
The source codes are available from the corresponding author on reasonable request.
References
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ (2020) The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395:912–920. https://doi.org/10.1016/S0140-6736(20)30460-8
Fiorillo A, Gorwood P (2020) The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry 63:e32. https://doi.org/10.1192/j.eurpsy.2020.35
Yao H, Chen JH, Xu YF (2020) Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 7:e21. https://doi.org/10.1016/S2215-0366(20)30090-0
Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM (2020) Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci 74:281–282. https://doi.org/10.1111/pcn.12988
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J (2020) The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 287:112934. https://doi.org/10.1016/j.psychres.2020.112934
Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C (2020) A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 87:40–48. https://doi.org/10.1016/j.bbi.2020.04.028
Fernández-Aranda F, Casas M, Claes L, Bryan DC, Favaro A, Granero R, Gudiol C, Jiménez-Murcia S, Karwautz A, Le Grange D, Menchón JM, Tchanturia K, Treasure J (2020) COVID-19 and implications for eating disorders. Eur Eat Disord Rev 28:239–245. https://doi.org/10.1002/erv.2738
Kavoor A (2020) COVID-19 in People with mental illness: challenges and vulnerabilities. Asian J Psychiatr 51:102051. https://doi.org/10.1016/j.ajp.2020.102051
Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, Pham LV, Tran KV, Duong TT, Tran TV, Duong TH, Nguyen TT, Nguyen QH, Hoang TM, Nguyen KT, Pham TTM, Yang SH, Chao JC, Duong TV (2020) People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med 9:965. https://doi.org/10.3390/jcm9040965
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 33:e100213. https://doi.org/10.1136/gpsych-2020-100213.Erratum.In:GenPsychiatr.2020Apr27;33(2):e100213corr1
Liu Y, Gayle AA, Wilder-Smith A, Rocklöv J (2020) The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med 27:taaa021. https://doi.org/10.1093/jtm/taaa021
Li S, Wang Y, Xue J, Zhao N, Zhu T (2020) The impact of COVID-19 epidemic declaration on psychological consequences: a study on active weibo users. Int J Env Res Public Health 17:2032. https://doi.org/10.3390/ijerph17062032
Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, Mytton O, Bonell C, Booy R (2020) School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health 4:397–404. https://doi.org/10.1016/S2352-4642(20)30095-X
MIUR. Available at: https://dati.istruzione.it/opendata/esploraidati. Accessed 30 Jul 2020
Wang G, Zhang Y, Zhao J, Zhang J, Jiang F (2020) Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395:945–947. https://doi.org/10.1016/S0140-6736(20)30547-X
Dalle Grave R (2020) Coronavirus disease 2019 and eating disorders. Eating disorders: The facts. Available at: https://www.psychologytoday.com/us/blog/eating-disorders-the-facts/202003/coronavirus-disease-2019- and-eating-disorders. Accessed 30 july 2021
Murphy R, Calugi S, Cooper Z, Dalle Grave R (2020) Challenges and opportunities for enhanced cognitive behaviour therapy (CBT-E) in light of COVID-19. Cogn Behav Therap 13:e14. https://doi.org/10.1017/S1754470X20000161
Touyz S, Lacey H, Hay P (2020) Eating disorders in the time of COVID-19. J Eat Disord 8:19. https://doi.org/10.1186/s40337-020-00295-3
Weissman RS, Klump KL, Wade T, Thomas JJ, Frank G, Waller G (2020) IJED support for eating disorders research in the time of COVID-19. Int J Eat Disord 53:1017–1020. https://doi.org/10.1002/eat.23293
Treasure J, Duarte TA, Schmidt U (2020) Eating disorders. Lancet 395:899–911. https://doi.org/10.1016/S0140-6736(20)30059-3
Hornberger LL, Lane MA, Committee On Adolescence (2021) Identification and management of eating disorders in children and adolescents. Pediatrics 147:e2020040279. https://doi.org/10.1542/peds.2020-040279
Ornstein RM, Katzman DK (2014) Child and adolescent feeding and eating disorders and the DSM-5: a brave new world. Adolesc Med State Art Rev 25:360–376
Ornstein RM, Rosen DS, Mammel KA, Callahan ST, Forman S, Jay MS, Fisher M, Rome E, Walsh BT (2013) Distribution of eating disorders in children and adolescents using the proposed DSM-5 criteria for feeding and eating disorders. J Adolesc Health 53:303–305. https://doi.org/10.1016/j.jadohealth.2013.03.025
Call C, Walsh BT, Attia E (2013) From DSM-IV to DSM-5: changes to eating disorder diagnoses. Curr Opin Psychiatry 26:532–536. https://doi.org/10.1097/YCO.0b013e328365a321
Solmi F, Downs JL, Nicholls DE (2021) COVID-19 and eating disorders in young people. Lancet Child Adolesc Health 5:316–318. https://doi.org/10.1016/S2352-4642(21)00094-8
Haripersad YV, Kannegiesser-Bailey M, Morton K, Skeldon S, Shipton N, Edwards K, Newton R, Newell A, Stevenson PG, Martin AC (2021) Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child 106:e15. https://doi.org/10.1136/archdischild-2020-319868
DSM-5. Section II. Diagnostic criteria and codes. Feeding and eating disorders. Available at: https://dsm.psychiatryonline.orghttps://doi.org/10.1176/appi.books.9780890425596.dsm10. Accessed 2 Oct 2021
Spettigue W, Obeid N, Erbach M, Feder S, Finner N, Harrison ME, Isserlin L, Robinson A, Norris ML (2021) The impact of COVID-19 on adolescents with eating disorders: a cohort study. J Eat Disord 9:65. https://doi.org/10.1186/s40337-021-00419-3
Zanna V, Cinelli G, Criscuolo M, Caramadre AM, Castiglioni MC, Chianello I, Marchili MR, Casamento Tumeo C, Guolo S, Tozzi AE, Vicari S (2021) Corrigendum: improvements on clinical status of adolescents with anorexia nervosa in inpatient and day hospital treatment: a retrospective pilot study. Front Psychiatry 12:748046. https://doi.org/10.3389/fpsyt.2021.748046.Erratumfor:FrontPsychiatry.2021May,28(12),pp.653482
Maria Monteleone A, Mereu A, Cascino G, Ruzzi V, Castiglioni MC, Patriciello G, Criscuolo M, Pellegrino F, Vicari S, Zanna V (2021) The validity of the fifth and the 10th Body Mass Index percentile as weight cut-offs for anorexia nervosa in adolescence: No evidence from quantitative and network investigation of psychopathology. Eur Eat Disord Rev 29:232–244. https://doi.org/10.1002/erv.2814
Otto AK, Jary JM, Sturza J, Miller CA, Prohaska N, Bravender T, Van Huysse J (2021) Medical admissions among adolescents with eating disorders during the COVID-19 pandemic. Pediatrics 148:e2021052201. https://doi.org/10.1542/peds.2021-052201
Scarpellini F, Segre G, Cartabia M, Zanetti M, Campi R, Clavenna A, Bonati M (2021) Distance learning in Italian primary and middle school children during the COVID-19 pandemic: a national survey. BMC Public Health 21:1035. https://doi.org/10.1186/s12889-021-11026-x
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors conceived the study concept. GS, MR, MRM, UR and AV designed the study, were major contributors in writing the manuscript, contributed to the interpretation of the data, reviewed and revised the manuscript; MR performed statistical analysis; FF, GM, GT, BG, AC allowed for the acquisition of data, reviewed and revised the manuscript; AD, VZ, SV, AR and AV contributed to interpretation of data, reviewed and critically revised the manuscript for important intellectual content; AV coordinated the study. revised it critically for important intellectual content; All Authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval was granted by the Research Ethics Board at the Bambino Gesù Children's Hospital, IRCCS, Rome, Italy.
Consent to participate
The requirement for informed consent was waived because the study was retrospective.
Consent for publication
The requirement for informed consent was waived because the study was retrospective.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spina, G., Roversi, M., Marchili, M.R. et al. Psychiatric comorbidities and dehydration are more common in children admitted to the emergency department for eating disorders in the COVID-19 era. Eat Weight Disord 27, 2473–2480 (2022). https://doi.org/10.1007/s40519-022-01386-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01386-7