Abstract
Introduction
Damage control surgery (DCS) is a standardized treatment concept in severe abdominal injury. Despite its evident advantages, DCS bears the risk of substantial morbidity and mortality, due to open abdomen therapy (OAT). Thus, identifying the suitable patients for that approach is of utmost importance. Furthermore, little is known about the use of DCS and the related outcome, especially in blunt abdominal trauma.
Methods
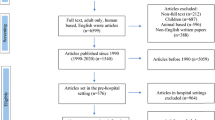
Patients recorded in the TraumaRegister DGU® from 2008 to 2017, and with an Injury Severity Score (ISS) ≥ 9 and an abdominal injury with an Abbreviated Injury Scale (AIS) score ≥ 3 were included in that registry-based analysis. Patients with DCS and temporary abdominal closure (TAC) were compared with patients who were treated with a laparotomy and primary closure (non-DCS) and those who did receive non-operative management (NOM). Following descriptive analysis, a matched-pairs study was conducted to evaluate differences and outcomes between DCS and non-DCS group. Matching criteria were age, abdominal trauma severity, and hemodynamical instability at the scene.
Results
The injury mechanism was predominantly blunt (87.1%). Of the 8226 patients included, 2351 received NOM, 5011 underwent laparotomy and primary abdominal closure (non-DCS), and 864 were managed with DCS. Thus, 785 patient pairs were analysed. The rate of hepatic injuries AIS > 3 differed between the groups (DCS 50.3% vs. non-DCS 18.1%). DCS patients had a higher ISS (p = 0.023), required more significant volumes of fluids, more catecholamines, and transfusions (p < 0.001). More DCS patients were in shock at the accident scene (p = 0.022). DCS patients had a higher number of severe hepatic (AIS score ≥ 3) and gastrointestinal injuries and more vascular injuries. Most severe abdominal injuries in non-DCS patients were splenic injuries (AIS, 4 and 5) (52.1% versus 37.9%, p = 0.004).
Conclusion
DCS is a strategy used in unstable trauma patients, severe hepatic, gastrointestinal, multiple abdominal injuries, and mass transfusions. The expected survival rates were achieved in such extreme trauma situations.



Similar content being viewed by others
Availability of data and material
Datasheets and analysis are made available upon request to the corresponding author.
Code availability
Not applicable.
References
Pfeifer R, Tarkin IS, Rocos B, Pape HC (2009) Patterns of mortality and causes of death in polytrauma patients–has anything changed? Injury 40(9):907–911. https://doi.org/10.1016/j.injury.2009.05.006
Burlew CC (2012) The open abdomen: practical implications for the practicing surgeon. Am J Surg 204(6):826–835. https://doi.org/10.1016/j.amjsurg.2012.04.013
Coccolini F, Biffl W, Catena F, Ceresoli M, Chiara O, Cimbanassi S, Fattori L, Leppaniemi A, Manfredi R, Montori G, Pesenti G, Sugrue M, Ansaloni L (2015) The open abdomen, indications, management and definitive closure. World J Emerg Surg 10:32. https://doi.org/10.1186/s13017-015-0026-5
Diaz JJ Jr, Cullinane DC, Dutton WD, Jerome R, Bagdonas R, Bilaniuk JW, Collier BR, Como JJ, Cumming J, Griffen M, Gunter OL, Kirby J, Lottenburg L, Mowery N, Riordan WP Jr, Martin N, Platz J, Stassen N, Winston ES (2010) The management of the open abdomen in trauma and emergency general surgery: part 1-damage control. J Trauma 68(6):1425–1438. https://doi.org/10.1097/TA.0b013e3181da0da5
Duff JH, Moffat J (1981) Abdominal sepsis managed by leaving abdomen open. Surgery 90(4):774–778
Open Abdomen Advisory P, Campbell A, Chang M, Fabian T, Franz M, Kaplan M, Moore F, Reed RL, Scott B, Silverman R (2009) Management of the open abdomen: from initial operation to definitive closure. Am Surg 75(11 Suppl):S1-22
Asensio JA, McDuffie L, Petrone P, Roldan G, Forno W, Gambaro E, Salim A, Demetriades D, Murray J, Velmahos G, Shoemaker W, Berne TV, Ramicone E, Chan L (2001) Reliable variables in the exsanguinated patient which indicate damage control and predict outcome. Am J Surg 182(6):743–751
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR, 3rd, Fruchterman TM, Kauder DR, Latenser BA, Angood PA (1993) ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 35 (3):375–382; discussion 382–373
Schwab CW (2004) Introduction: damage control at the start of 21st century. Injury 35(7):639–641. https://doi.org/10.1016/j.injury.2004.03.001
Shapiro MB, Jenkins DH, Schwab CW, Rotondo MF (2000) Damage control: collective review. J Trauma 49(5):969–978
Chiara O, Cimbanassi S, Biffl W, Leppaniemi A, Henry S, Scalea TM, Catena F, Ansaloni L, Chieregato A, de Blasio E, Gambale G, Gordini G, Nardi G, Paldalino P, Gossetti F, Dionigi P, Noschese G, Tugnoli G, Ribaldi S, Sgardello S, Magnone S, Rausei S, Mariani A, Mengoli F, di Saverio S, Castriconi M, Coccolini F, Negreanu J, Razzi S, Coniglio C, Morelli F, Buonanno M, Lippi M, Trotta L, Volpi A, Fattori L, Zago M, de Rai P, Sammartano F, Manfredi R, Cingolani E (2016) International consensus conference on open abdomen in trauma. J Trauma Acute Care Surg 80(1):173–183. https://doi.org/10.1097/TA.0000000000000882
Hsu JM, Pham TN (2011) Damage control in the injured patient. Int J Crit Illn Inj Sci 1(1):66–72. https://doi.org/10.4103/2229-5151.79285
Hommes M, Chowdhury S, Visconti D, Navsaria PH, Krige JEJ, Cadosch D, Nicol AJ (2018) Contemporary damage control surgery outcomes: 80 patients with severe abdominal injuries in the right upper quadrant analyzed. Eur J Trauma Emerg Surg 44(1):79–85. https://doi.org/10.1007/s00068-017-0768-8
Ordonez CA, Pino LF, Badiel M, Sanchez AI, Loaiza J, Ballestas L, Puyana JC (2011) Safety of performing a delayed anastomosis during damage control laparotomy in patients with destructive colon injuries. J Trauma 71 (6):1512–1517; discussion 1517–1518. https://doi.org/10.1097/TA.0b013e31823d0691
Roberts DJ, Bobrovitz N, Zygun DA, Kirkpatrick AW, Ball CG, Faris PD. Stelfox HD (2021) Evidence for use of damage control surgery and damage control interventions in civilian trauma patients: a systematic review. World J Emerg Surg. https://doi.org/10.1186/s13017-021-00352-5
Willms AG, Schaaf S, Zimmermann N, Schwab R, Gusgen C, Vilz TO, Kalff JC, von Websky MW (2019) The significance of visceral protection in preventing enteroatmospheric fistulae during open abdomen treatment in patients with secondary peritonitis: a propensity score-matched case-control analysis. Ann Surg. https://doi.org/10.1097/SLA.0000000000003440
Bruhin A, Ferreira F, Chariker M, Smith J, Runkel N (2014) Systematic review and evidence based recommendations for the use of negative pressure wound therapy in the open abdomen. Int J Surg 12(10):1105–1114. https://doi.org/10.1016/j.ijsu.2014.08.396
Atema JJ, Gans SL, Boermeester MA (2015) Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg 39(4):912–925. https://doi.org/10.1007/s00268-014-2883-6
Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E, Kluger Y, Moore EE, Coimbra R, Kirkpatrick AW, Pereira BM, Montori G, Ceresoli M, Abu-Zidan FM, Sartelli M, Velmahos G, Fraga GP, Leppaniemi A, Tolonen M, Galante J, Razek T, Maier R, Bala M, Sakakushev B, Khokha V, Malbrain M, Agnoletti V, Peitzman A, Demetrashvili Z, Sugrue M, Di Saverio S, Martzi I, Soreide K, Biffl W, Ferrada P, Parry N, Montravers P, Melotti RM, Salvetti F, Valetti TM, Scalea T, Chiara O, Cimbanassi S, Kashuk JL, Larrea M, Hernandez JAM, Lin HF, Chirica M, Arvieux C, Bing C, Horer T, De Simone B, Masiakos P, Reva V, DeAngelis N, Kike K, Balogh ZJ, Fugazzola P, Tomasoni M, Latifi R, Naidoo N, Weber D, Handolin L, Inaba K, Hecker A, Kuo-Ching Y, Ordonez CA, Rizoli S, Gomes CA, De Moya M, Wani I, Mefire AC, Boffard K, Napolitano L, Catena F (2018) The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 13:7. https://doi.org/10.1186/s13017-018-0167-4
Lopez-Cano M, Garcia-Alamino JM, Antoniou SA, Bennet D, Dietz UA, Ferreira F, Fortelny RH, Hernandez-Granados P, Miserez M, Montgomery A, Morales-Conde S, Muysoms F, Pereira JA, Schwab R, Slater N, Vanlander A, Van Ramshorst GH, Berrevoet F (2018) EHS clinical guidelines on the management of the abdominal wall in the context of the open or burst abdomen. Hernia 22(6):921–939. https://doi.org/10.1007/s10029-018-1818-9
Cristaudo A, Jennings S, Gunnarsson R, DeCosta A (2017) Complications and mortality associated with temporary abdominal closure techniques: a systematic review and meta-analysis. Am Surg 83(2):191–216
Becker HP, Willms A, Schwab R (2007) Small bowel fistulas and the open abdomen. Scand J Surg 96(4):263–271. https://doi.org/10.1177/145749690709600402
Barker DE, Kaufman HJ, Smith LA, Ciraulo DL, Richart CL, Burns RP (2000) Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma 48 (2):201–206; discussion 206–207
Willms A, Gusgen C, Schaaf S, Bieler D, von Websky M, Schwab R (2015) Management of the open abdomen using vacuum-assisted wound closure and mesh-mediated fascial traction. Langenbecks Arch Surg 400(1):91–99. https://doi.org/10.1007/s00423-014-1240-4
Salamone G, Licari L, Guercio G, Comelli A, Mangiapane M, Falco N, Tutino R, Bagarella N, Campanella S, Porrello C, Gullo R, Cocorullo G, Gulotta G (2018) Vacuum-assisted wound closure with mesh-mediated fascial traction achieves better outcomes than vacuum-assisted wound closure alone: a comparative study. World J Surg 42(6):1679–1686. https://doi.org/10.1007/s00268-017-4354-3
Acosta S, Bjarnason T, Petersson U, Palsson B, Wanhainen A, Svensson M, Djavani K, Bjorck M (2011) Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg 98(5):735–743. https://doi.org/10.1002/bjs.7383
Smith J, Caldwell E, D’Amours S, Jalaludin B, Sugrue M (2005) Abdominal trauma: a disease in evolution. ANZ J Surg 75(9):790–794. https://doi.org/10.1111/j.1445-2197.2005.03524.x
Beale EW, Janis JE, Minei JP, Elliott AC, Phelan HA (2013) Predictors of failed primary abdominal closure in the trauma patient with an open abdomen. South Med J 106(5):327–331. https://doi.org/10.1097/SMJ.0b013e31829243ed
Cirocchi RBA, Biffl WL, Mutafchiyski V, Popivanov G, Chiara O, Tugnoli G, Di Saverio S (2016) What is the effectiveness of the negative pressure wound therapy (NPWT) in patients treated with open abdomen technique? A systematic review and meta-analysis. J Trauma Acute Care Surg 81(3):575–584
Gennarelli TA, Wodzin E (2006) AIS 2005: a contemporary injury scale. Injury 37(12):1083–1091. https://doi.org/10.1016/j.injury.2006.07.009
Taylor P (2013) Standardized mortality ratios. Int J Epidemiol 42(6):1882–1900. https://doi.org/10.1093/ije/dyt209
Jensen KO, Teuben MPJ, Lefering R, Halvachizadeh S, Mica L, Simmen H, Pfeifer R, Pape H, Sprengel K, The TraumaRegister DGU (2021) Pre-hospital trauma care in Switzerland and Germany: do they speak the same language? Eur J Trauma Emerg Surg 47:1273–1280. https://doi.org/10.1007/s00068-020-01306-3
Baker SP, O’Neill B, Haddon W Jr, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14(3):187–196
Stoner HB, Heath DF, Yates DW, Frayn KN (1980) Measuring the severity of injury. J R Soc Med 73(1):19–22
Mikhail J (1999) The trauma triad of death: hypothermia, acidosis, and coagulopathy. AACN Clin Issues 10(1):85–94
Roberts DJ, Bobrovitz N, Zygun DA, Ball CG, Kirkpatrick AW, Faris PD, Brohi K, D’Amours S, Fabian TC, Inaba K, Leppaniemi AK, Moore EE, Navsaria PH, Nicol AJ, Parry N, Stelfox HT (2016) Indications for use of damage control surgery in civilian trauma patients: a content analysis and expert appropriateness rating study. Ann Surg 263(5):1018–1027. https://doi.org/10.1097/SLA.0000000000001347
Butcher N, Balogh ZJ (2009) The definition of polytrauma: the need for international consensus. Injury 40(Suppl 4):S12-22. https://doi.org/10.1016/j.injury.2009.10.032
Clancy TV, Gary Maxwell J, Covington DL, Brinker CC, Blackman D (2001) A statewide analysis of level I and II trauma centers for patients with major injuries. J Trauma 51(2):346–351. https://doi.org/10.1097/00005373-200108000-00021
Lefering R, Huber-Wagner S, Bouillon B, Lawrence T, Lecky F, Bouamra O (2020) Cross-validation of two prognostic trauma scores in severely injured patients. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-020-01373-6
Acknowledgements
We would like to thank the members of the Polytrauma Study Group of the German Trauma Society (DGU®) for their many years of hard work and commitment to TraumaRegister DGU®. In 2007, the Polytrauma Study Group was integrated into the Committee on Emergency Medicine, Intensive Care, and Trauma Management (Sektion NIS) of the German Trauma Society (DGU). We would also like to thank the German Office of Languages in Hürth for linguistic support. We thank the hospitals that contributed data to TraumaRegister DGU® for their commitment.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethics approval
The study was performed following the current publication guideline of the TraumaRegister DGU® and is registered as TR-DGU Project ID 2018–049. Since the study was a retrospective analysis based on aggregated routine data, ethical approval was not required according to the responsible regional medical association (Ethikkommission der Landesärztekammer Rheinland-Pfalz, Mainz, Germany). This study was registered in the German Clinical Trials Register (DRKS) in accordance with the ICMJE requirements (ID: DRKS00023988).
Consent to participate/consent to publication
Patients agreed on study participation and data publication as informed consent of entering the data into TraumaRegister DGU® has been obtained.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Willms, A., Güsgen, C., Schwab, R. et al. Status quo of the use of DCS concepts and outcome with focus on blunt abdominal trauma. Langenbecks Arch Surg 407, 805–817 (2022). https://doi.org/10.1007/s00423-021-02344-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02344-0