Abstract
Purpose
Uveal melanoma (UM) is an orphan cancer of high unmet medical need. Current patterns of care and surveillance remain unclear as they are situated in an interdisciplinary setting.
Methods
A questionnaire addressing the patterns of care and surveillance in the management of patients with uveal melanoma was distributed to 70 skin cancer centers in Austria, Germany and Switzerland. Frequency distributions of responses for each item of the questionnaire were calculated.
Results
44 of 70 (62.9%) skin cancer centers completed the questionnaire. Thirty-nine hospitals were located in Germany (88.6%), three in Switzerland (6.8%) and two in Austria (4.5%). The majority (68.2%) represented university hospitals. Most patients with metastatic disease were treated in certified skin cancer centers (70.7%, 29/41). Besides, the majority of patients with UM were referred to the respective skin cancer center by ophthalmologists (87.2%, 34/39). Treatment and organization of follow-up of patients varied across the different centers. 35.1% (14/37) of the centers stated to not perform any screening measures.
Conclusion
Treatment patterns of patients with uveal melanoma in Germany, Austria and Switzerland remain extremely heterogeneous. A guideline for the treatment and surveillance is urgently needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Ocular melanoma is a rare cancer condition that can develop as uveal or conjunctival tumors. Uveal melanoma (UM) represents one of the most common ocular malignancies among adults and accounts for about 5% of all melanoma cases. Primary tumors originate from the pigment cells of the choroid layer, the ciliary body or iris of the eye (Chattopadhyay et al. 2016). With an incidence of 4–7 cases per million in Europe, it is much rarer than cutaneous melanoma (Mallone et al. 2012). Therapeutic options of local disease include radiation therapies or surgical approaches like local resection and enucleation of the affected eye. Although these measures are highly effective to achieve local tumor control, up to 50% of patients develop distant metastases, which are mostly localized to liver and lungs (Bedikian 2006).
Risk for metastases strongly depends on monosomy 3 (Shields et al. 2011). Once UM becomes metastatic, the disease course is often aggressive and the prognosis is dismal with an average survival time of 1 year across all therapeutic regimens (Rantala et al. 2019). A combined approach with local treatment and combined immunotherapy has been employed with a median overall survival of 18 months in a small group of patients (Kirchberger et al. 2018). Thus, therapy options remain limited and have often been adopted from cutaneous melanoma, although these entities differ clinically and genetically (Heppt et al. 2017b). Few intervention studies have been published for UM and sound randomized controlled trials are lacking. Neither targeted therapy with MEK inhibitors nor immune checkpoint blockade (ICB) demonstrated significantly improvement of the prognosis of patients with UM (Heppt et al. 2017b; Steeb et al. 2018). Thus, creating a solid and uniform framework or guideline for evidence-based treatment decisions remains challenging.
The management of UM is subject to country-specific regulations. Currently, only a few international and consensus-based guidelines exist (Mathis et al. 2018; Nathan et al. 2015; Simpson et al. 2014; Weis et al. 2016), a German guideline is currently not yet available. Besides, the care of patients with UM is organized in an interdisciplinary setting, involving ophthalmologists, oncologists, interventional radiologists and dermato-oncologists. As current patterns of care are heterogeneous and the optimal management for patients with UM is yet to be determined, we performed a tri-national cross-sectional study to explore the current standard of care in German-speaking skin cancer centers.
Methods
As no validated survey existed for the objective of our study, the questionnaire with a total of 15 items was developed de-novo based on our institutional experience. The explorative survey included questions in a multiple-choice format regarding various treatment approaches for primary and metastatic disease of ocular melanoma [i.e., UM and conjunctival melanoma (CM)], follow-up of patients, as well as items related to interdisciplinary cooperation. The questionnaire was pre-tested by independent researchers for clarity and comprehension. Based on their suggestions, the questionnaire was revised to its final form. The full questionnaire is available upon request. We encouraged the centers to also reply to our survey in case that they had not seen any patients with UM in 2018.
The paper-based questionnaire was distributed via mail to 70 skin cancer centers in Germany, Austria and Switzerland on 6 August 2019. A reminding letter was sent to all non-responders prolonging the initially stated period for response from 2 up to 4 months to increase the response rate. Contact information of the 70 participating centers (69 certified skin cancer centers and one uncertified center) were obtained via OncoMap® by OnkoZert®, an independent institute by the German Cancer Society which is responsible for the inspection and certification of cancer centers and oncology centers in Germany, Austria, and Switzerland (https://www.onkozert.de/). Participation was voluntary and each center was allowed to participate only once in the survey (cross-sectional design). Answered questionnaires could be sent back via E-Mail, Fax, or regular mail.
Frequency distributions of responses for each item were calculated and reported descriptively as absolute values and percentages (%). Quantitative variables were expressed as median with ranges. Subgroup differences were explored with Mood’s Median-Test. A p-value of < 0.05 was considered as significant. Statistical analyses were conducted with SPSS (IBM SPSS Statistics version 25, IBM Corporation).
Results
Characteristics of the participating centers
Overall, 44 of 70 (62.9%) centers completed the questionnaire. Most of the responding centers were located in Germany (88.6%, n = 39), three were located in Switzerland (6.8%) and two in Austria (4.5%). The majority (68.2%, 30/44) represented university hospitals and one third municipal or private hospitals (31.8%, 14/44) (Fig. 1a).
a Geographical map of the responding certified skin cancer centers in Austria, Germany, and Switzerland, b bar chart illustrating the timepoint of UM and CM patients’ first presentation to the skin cancer center, and c pattern of UM and CM patients’ referral by multidisciplinary professions to the skin cancer centers
In 86.8% (33/38) of the centers, patients with UM or CM presented for the first time after histological confirmation of distant metastases, followed by presentation upon clinical or radiological suspicion of distant metastases in 83.8% (31/38). In nearly half of the centers (52.6%, 20/38), UM or CM patients presented after treatment of the primary ocular tumor (Fig. 1b).
Patients with UM or CM were referred by ophthalmologists (87.2%, 34/39), hematologists/oncologists (71.8%, 28/39), general practitioners (56.4%, 22/39), and radiologists (25.6%, 10/39) (Fig. 1c). Other professions mentioned in the free-text field included dermatologists (n = 3), patients themselves (n = 1), gastroenterologists (n = 1) or others (n = 3).
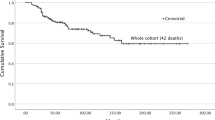
Surveillance
A total of 460 patients with primary UM were estimated to be treated at the skin cancer centers in 2018. 396 of these 460 patients with primary UM (86.1%) were treated in German skin cancer centers. The number of patients undergoing surveillance for UM at the skin cancer centers in 2018 ranged from 0 to 100 (median 3). Overall, 11.4% (5/44) of the participating centers did not have any patients in surveillance. Notably, more patients were followed-up on in a university hospital setting than in municipal or private hospitals (p = 0.013).
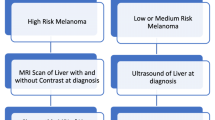
Surveillance of uveal melanoma (stages I–IIIC)
Half of the centers (51.4%, 19/37) performed regular screening measures to detect metastatic disease after the primary diagnosis of UM in case of a high-risk profile, such as large primary tumor or high vertical tumor thickness. Screening due to a high molecular risk profile such as monosomy 3 was performed in 32.4% (12/37). In contrast, 35.1% (14/37) did not perform any screening measures. The surveillance was exclusively performed by ophthalmology departments in three centers.
When asked about the specific screening and diagnostic measures performed during follow-up care, 76.3% (29/38) reported liver sonography, followed by total-body examination (63.2%, 24/38), magnetic resonance imaging (MRI) (52.6%, 20/38), computed tomography (CT) scans (47.4%, 18/38) and positron emission tomography–computed tomography (PET-CT) (21.1%, 8/38) (Fig. 2a). Other modalities were lymph node sonography (n = 3) and chest x-ray (n = 2).
Bar chart illustrating a the deployed screening measures in the skin cancer centers for patients with UM b applied screening intervals in different years of follow-up for UM. Abbreviations: CT: computed tomography, PET-CT: positron emission tomography–computed tomography, MRI: magnetic resonance imaging, MIA: melanoma inhibitory antigen, LDH: lactate dehydrogenase
Other screening measures stated in a free-text field comprised the assessment of serum biomarkers including S100 (n = 4), melanoma inhibitory activity protein (MIA, n = 2), liver enzymes (n = 1), lactate dehydrogenase (LDH, n = 2) or tumor markers in general (n = 1). One center had no uniform guidelines but performed regular sonography or MRI of the liver. Another one adapted the recommendations for the follow-up of stage III cutaneous melanoma.
The majority performed follow-up examinations at intervals of 3 months (66.7%, 22/33) or 6 months (51.5%, 17/33). Besides, three centers conducted surveillance at intervals of 12 months (9.1%), while one stated that intervals were longer than 12 months. No specific intervals were reported by three centers. Twenty-one centers provided more information about the screening intervals in different years of follow-up (Fig. 2b). The screening intervals differed between centers especially when the time of follow-up was longer than 3 years. Twelve centers also provided detailed information about distinct screening measurements and intervals (Table 1).
Management of metastatic disease
Overall, 249 patients with metastatic UM (median: 3, range 0–50) were treated in 2018 in the participating centers. The median significantly differed between university and municipal hospitals (p = 0.003), i.e., more patients with metastatic disease were followed-up on in university hospitals.
Most patients with metastatic disease (UM and CM) were treated in the skin cancer centers or dermatology departments (70.7%, 29/41), while 12.2% (5/41) indicated that patients were treated in hematology/oncology units only. In 5 centers (12.2%), patients with metastatic disease were treated both by skin cancer centers and hematology/oncology units. One center reported simultaneous treatment in the ophthalmology and gastroenterology departments, respectively. In one center, patients with metastatic disease were treated in the gastroenterology department.
We also investigated which systemic treatments were applied for metastatic UM in 2018. Nearly 80% of centers (35/40) applied nivolumab in combination with ipilimumab, followed by conventional chemotherapy (50%, 20/40), nivolumab monotherapy (42.5%, 17/40), and pembrolizumab monotherapy (40%, 16/40) (Fig. 3a). Besides, MEK inhibitors and ipilimumab monotherapy were applied in 35% (14/40) and 15% (6/40), respectively. Other treatments mentioned in a free-text field included tebentafusp (n = 5), sorafenib (n = 4) and cabozantinib (n = 1), BRAF plus MEK inhibitor (n = 1), dendritic cell vaccination (n = 1), and talimogene laherparepvec (n = 1).
Bar charts illustrating a available systemic treatments in the skin cancer centers and b liver-directed approaches for the management of metastatic UM and CM. Abbreviations: DC: dendritic cell, T-VEC: talimogene laherparepvec, SIRT: selective internal radiation therapy, RFA: radiofrequency ablation, TACE: trans-arterial chemoembolization
As UM has a unique propensity for metastatic spread to the liver, we specifically investigated liver-directed treatments (Collaborative Ocular Melanoma Study 2001). Selective internal radiation therapy (SIRT) was most frequently performed (79.4%; 27/34), followed by radiofrequency ablation (RFA) with 58.8% (20/34), trans-arterial chemoembolization (TACE) (55.9%, 19/34), and stereotactic radiation (50%, 17/34) (Fig. 3b).
Implications and unmet needs
At the end of the questionnaire, all responders were invited to raise general comments or wishes regarding the management of UM. Most desired clear follow-up schemes for the surveillance of tumor-free patients with UM. Surveillance, especially regarding intervals and duration of follow-up, is currently not yet standardized, but rather individual. Guidelines are, therefore, desirable as currently treatment of patients with UM is mostly based on individual experience. Additionally, a central register for patients with ocular melanoma was suggested by one center.
Discussion
Uveal melanoma is a rare cancer condition of high unmet clinical need. The aim of our survey was to provide an overview of the current patterns of care and surveillance in German-speaking skin cancer centers. We focused on skin cancer centers as the treatment of metastatic disease is currently mostly performed in analogy to cutaneous melanoma including checkpoint blockade and kinase inhibitors. Not surprisingly, more patients were treated in follow-up care at university hospitals compared to municipal hospitals. In 2016, 642 adult patients were newly diagnosed with ocular cancer (ICD-10 C69) in Germany, indicating that the skin cancer centers represented in our survey treated approximately more than 70% of all newly diagnosed cases (Robert Koch-Institut 2020). Taking into account that up to 50% of all patients with UM develop distant metastases (Bedikian 2006) approximately 320 patients in Germany will be diagnosed with metastatic disease per year. In our survey, the skin cancer centers stated to care for 253 patients, indicating that in Germany, almost 80% of all patients with metastatic ocular melanoma, i.e., UM or CM, are treated in these departments. These numbers highlight the importance of skin cancer centers for the therapy and surveillance of patients with both primary and metastatic ocular melanoma.
Although UM differs from cutaneous melanoma both clinically and biologically, treatment options for advanced stages have largely been adopted from it, yet with much lower response rates and at the cost of high treatment-related toxicity (Heppt et al. 2017a, 2019). This makes it difficult to demonstrate the clinical effectiveness of interventions and to create a solid framework for evidence-based treatment decisions. Our survey among skin cancer centers in Germany, Austria and Switzerland confirmed the urgent need for the development of clinical practice guidelines for this rare cancer entity, comparable to other consortia (Mathis et al. 2018; Nathan et al. 2015; Simpson et al. 2014; Weis et al. 2016). Special strategies need to be employed to generate evidence that is compatible with rigorous quality standards of guidelines (Pai et al. 2019). Previous assessments of the methodological quality of international guidelines on UM have identified weaknesses and strengths of existing guidelines which require particular attention and improvement in future guidelines (Steeb et al. 2020). A guideline from the United Kingdom published by Nathan et al. was rated as best and may hence serve as a basis for a future German guideline.
A further barrier towards the management of UM comes from the fact that the care of patients with UM occurs in a highly interdisciplinary setting, involving ophthalmologists, hematologists, oncologists, interventional radiologists and dermato-oncologists. This highlights the urgent need for an interdisciplinary guideline. For patients with primary disease, mostly ophthalmologists and radiation oncologists are involved in the care, while patients with metastatic disease are often referred to dermato-oncologists, which is in line with our sample. The majority of surveyed responders stated that patients presented to their center after the histological confirmation of distant metastases. Thus, ICB is often adopted as therapeutic strategy from cutaneous melanoma with 80% of centers treating metastatic patients with nivolumab plus ipilimumab. Beside the broad usage of ICB, chemotherapy was also often applied although it has only limited efficacy irrespective of the chemotherapeutic agent (Carvajal et al. 2017). This underlines that novel treatment strategies are utterly needed. Clinical studies investigating new treatment options as, e.g., tebentafusp (IMCgp100), a bispecific protein bridging CD3 + T cells and gp100-expressing tumor cells (Liddy et al. 2012) have shown promising results in phase I/II trials so far (Carvajal et al. 2018; Middleton et al. 2016).
Screening and follow-up of patients varied the most across our sample. Some followed the evidence- and consensus-based guideline for stage III cutaneous melanoma (Eigentler et al. 2017), while others based their follow-up schedule on the recommendations established within their institution or on personal experience. This highlights again the urgent need for uniform recommendations which should be based on progression and recurrence rate.
There are several limitations of this study. The response rate was limited to 44 of 70 skin cancer centers. Besides this, university hospitals were overrepresented, thus diminishing the overall representability of the results. Furthermore, recall bias may be likely as the participating centers had to remember management of patients of the years before. Additionally, in some items, the answers of the participants differed extremely for instance when reporting the follow-up schemes, ranging from only brief descriptions to detailed reports including follow-up intervals and screening methods. However, to the best of our knowledge, practice and surveillance patterns in German-speaking countries have not been investigated so far, and therefore, our results represent a first step towards standardized care for patients with ocular melanoma.
Our results will contribute to improve nationwide management of ocular melanoma and to deduce possible future projects within the German Dermatologic Cooperative Oncology Group (DeCOG).
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Code availability
SPSS Statistics version 25 (IBM Corporation, Armonk, NY, USA) was used to analyze the data.
References
Bedikian AY (2006) Metastatic uveal melanoma therapy: current options. Int Ophthalmol Clin 46:151–166. https://doi.org/10.1097/01.iio.0000195852.08453.de
Carvajal RD et al (2018) Safety, efficacy and biology of the gp100 TCR-based bispecific T cell redirector IMCgp100 in advanced uveal melanoma. Invest Ophthalmol Vis Sci 59:3622–3622
Carvajal RD, Schwartz GK, Tezel T, Marr B, Francis JH, Nathan PD (2017) Metastatic disease from uveal melanoma: treatment options and future prospects. Br J Ophthalmol 101:38–44. https://doi.org/10.1136/bjophthalmol-2016-309034
Chattopadhyay C et al (2016) Uveal melanoma: From diagnosis to treatment and the science in between. Cancer 122:2299–2312. https://doi.org/10.1002/cncr.29727
Collaborative Ocular Melanoma Study G (2001) Assessment of metastatic disease status at death in 435 patients with large choroidal melanoma in the Collaborative Ocular Melanoma Study (COMS): COMS report no. 15. Arch Ophthalmol 119:670–676. https://doi.org/10.1001/archopht.119.5.670
Eigentler TK, Muhlenbein C, Follmann M, Schadendorf D, Garbe C (2017) S3-Leitlinie Diagnostik, Therapie und Nachsorge des Melanoms - Update 2015/2016, Kurzversion 2.0. J Dtsch Dermatol Ges 15:e1–e41. https://doi.org/10.1111/ddg.13247
Heppt MV et al (2019) Combined immune checkpoint blockade for metastatic uveal melanoma: a retrospective, multi-center study. J Immunother Cancer 7:299. https://doi.org/10.1186/s40425-019-0800-0
Heppt MV et al (2017a) Prognostic factors and outcomes in metastatic uveal melanoma treated with programmed cell death-1 or combined PD-1/cytotoxic T-lymphocyte antigen-4 inhibition. Eur J Cancer 82:56–65. https://doi.org/10.1016/j.ejca.2017.05.038
Heppt MV et al (2017b) Immune checkpoint blockade for unresectable or metastatic uveal melanoma: A systematic review. Cancer Treat Rev 60:44–52. https://doi.org/10.1016/j.ctrv.2017.08.009
Kirchberger MC, Moreira A, Erdmann M, Schuler G, Heinzerling L (2018) Real world experience in low-dose ipilimumab in combination with PD-1 blockade in advanced melanoma patients. Oncotarget 9:28903–28909. https://doi.org/10.18632/oncotarget.25627
Liddy N et al (2012) Monoclonal TCR-redirected tumor cell killing. Nat Med 18:980–987. https://doi.org/10.1038/nm.2764
Mallone S et al (2012) Descriptive epidemiology of malignant mucosal and uveal melanomas and adnexal skin carcinomas in Europe. Eur J Cancer 48:1167–1175. https://doi.org/10.1016/j.ejca.2011.10.004
Mathis T et al (2018) Management of uveal melanomas, guidelines for oncologists. Bull Cancer 105:967–980. https://doi.org/10.1016/j.bulcan.2018.07.011
Middleton MR et al (2016) Safety, pharmacokinetics and efficacy of IMCgp100, a first-in-class soluble TCR-antiCD3 bispecific t cell redirector with solid tumour activity: Results from the FIH study in melanoma. J Clin Oncol 34:3016–3016. https://doi.org/10.1200/JCO.2016.34.15_suppl.3016
Nathan P et al (2015) Uveal Melanoma UK National Guidelines. Eur J Cancer 51:2404–2412. https://doi.org/10.1016/j.ejca.2015.07.013
Pai M et al (2019) Strategies for eliciting and synthesizing evidence for guidelines in rare diseases. BMC Med Res Methodol 19:67. https://doi.org/10.1186/s12874-019-0713-0
Rantala ES, Hernberg M, Kivela TT (2019) Overall survival after treatment for metastatic uveal melanoma: a systematic review and meta-analysis. Melanoma Res 29:561–568. https://doi.org/10.1097/CMR.0000000000000575
Robert Koch-Institut Zentrum für Krebsregisterdaten im Robert Koch-Institut: Datenbankabfrage mit Schätzung der Inzidenz, Prävalenz und des Überlebens von Krebs in Deutschland auf Basis der epidemiologischen Landeskrebsregisterdaten https://doi.org/10.18444/5.03.01.0005.0014.0001). Mortalitätsdaten bereitgestellt vom Statistischen Bundesamt. Available from: www.krebsdaten.de/abfrage (Accessed 22.06.2020)
Shields CL, Ganguly A, Bianciotto CG, Turaka K, Tavallali A, Shields JA (2011) Prognosis of uveal melanoma in 500 cases using genetic testing of fine-needle aspiration biopsy specimens. Ophthalmology 118:396–401. https://doi.org/10.1016/j.ophtha.2010.05.023
Simpson ER et al (2014) The American Brachytherapy Society consensus guidelines for plaque brachytherapy of uveal melanoma and retinoblastoma. Brachytherapy 13:1–14. https://doi.org/10.1016/j.brachy.2013.11.008
Steeb T et al (2020) Guidelines for uveal melanoma: a critical appraisal of systematically identified guidelines using the AGREE II and AGREE-REX instrument. J Cancer Res Clin Oncol 146:1079–1088. https://doi.org/10.1007/s00432-020-03141-w
Steeb T, Wessely A, Ruzicka T, Heppt MV, Berking C (2018) How to MEK the best of uveal melanoma: A systematic review on the efficacy and safety of MEK inhibitors in metastatic or unresectable uveal melanoma. Eur J Cancer 103:41–51. https://doi.org/10.1016/j.ejca.2018.08.005
Weis E et al (2016) Management of uveal melanoma: a consensus-based provincial clinical practice guideline. Curr Oncol 23:e57-64. https://doi.org/10.3747/co.23.2859
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Steeb, T., Wessely, A., Alter, M. et al. Patterns of care and follow-up care of patients with uveal melanoma in German-speaking countries: a multinational survey of the German Dermatologic Cooperative Oncology Group (DeCOG). J Cancer Res Clin Oncol 147, 1763–1771 (2021). https://doi.org/10.1007/s00432-020-03450-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03450-0