Abstract
Purpose
To evaluate the effect around nurses’ shift change and on-call physicians’ shift change on obstetrical outcomes.
Methods
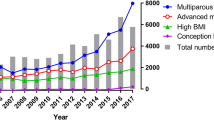
A retrospective study of women who had an attempt of labor in a single-medical center, January 2006–December 2017. Obstetrical outcomes were compared between the time around nurses’ shift change (6:00–8:00, 14:00–16:00, and 22:00–00:00) to the rest of the day, and between the time around on-call physicians’ shift change (6:00–8:00, 14:00–16:00) to the rest of the day.
Results
32,861 women were included, 7826 deliveries occurred during nurses’ shift-change, and 25,035 deliveries occurred during the rest of the day. The groups had similar general and obstetrical characteristics, with no statistical difference in cesarean delivery rate (10% vs. 9.8%, P = 0.45) (Table 1). Nurses’ shift change had no measurable effect on obstetrical outcomes, including induction of labor, preterm labor, 5-min-Apgar score and cord pH value, except PPH which was less likely to occur during nurses’ shift change period (3.8% vs. 4.4%, P = 0.045) (Table 2). From 32,861 deliveries, 5155 deliveries occurred during on-call physicians’ shift-change, and 27,706 deliveries occurred during the rest of the day. Induction\augmentation of labor and epidural analgesia were less likely to happen during on-call physicians’ shift change (34.4% vs. 38%, P < 0.0001, 59.6% vs. 61.8%, P = 0.003, respectively) (Table 3). The two groups had similar obstetrical outcomes, without statistical difference in cesarean delivery rate (10% vs. 9.8%, P = 0.63) (Table 4).
Conclusion
Nurses’ shift change and on-call physicians’ shift change does not appear to be associated with an increase in adverse maternal or neonatal outcomes.
Similar content being viewed by others
References
Duncan Jha AK, Bates BW (2001) Fatigue, sleepiness, and medical errors. In: Shojania KG, Duncan BW, Mcdonald KM, Wachter RM (eds) Making health care safer: A critical analysis of patient safety practices. Agency for Healthcare Research and Quality, United States Department of Health and Human Services, Rockville
Rogers AE (2008) The Effects of fatigue and sleepiness on nurse performance and patient safety. In: Hughes RG (ed) Patient safety and quality: an evidence-based handbook for nurses. MD Agency for Healthcare Research and Quality, Rockville
Landrigan CP, Rothschild JM, Cronin JW et al (2004) Effect of reducing intern's work hours on serious medical errors in intensive care units. N Engl J Med 351:1838–1848
Barger LK, Ayas NT, Cade BE et al (2006) Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med 3:e487
The Joint Commission (2011) Sentinel event alert: health care worker fatigue and patient safety. Sentinel Event Alerts, issue 48. The Joint Commission
Mccormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE (2012) Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg 147:430–435
Smith-Miller CA, Shaw-Kokot J, Curro B, Jones CB (2014) An integrative review: fatigue among nurses in acute care settings. J Nurs Adm 44:487–494
Mansukhani MP, Kolla BP, Surani S, Varon J, Ramar K (2012) Sleep deprivation in resident s, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med 124:241–249
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH (1994) Does house staff discontinuity of care increase the risk for preventable adverse events? [comment]. Ann Intern Med 121:866–872
Chelmow D, O’Brian B (2006) Postpartum haemorrhage: prevention. Clin Evid 2006:1932–1950
Myles TD, Santolaya J (2003) Maternal and neonatal outcomes in patients with a prolonged second stage of labor. Obstet Gynecol 102:52–58
Cheng YW, Hopkins LM, Laros RK Jr, Caughey AB (2007) Duration of the second stage of labor in multiparous women: maternal and neonatal outcomes. Am J Obstet Gynecol 196:e1–6
Bailit JL, Landon MB, Lai Y, Rouse DJ, Spong CY, Varner MW, Moawad AH, Simhan HN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Jo O’Sullivan M, Sibai BM, Langer O (2008) Maternal-Fetal Medicine Units Network Cesarean Registry: impact of shift change on cesarean complications Am. J Obstetr Gynecol 198(2):173.e1–173.e5. https://doi.org/10.1016/j.ajog.2007.11.003
Reichman O, Samueloff A, Gdansky E, Yekel Y, Calderon-Margalit R (2015) Delivery during time of shift change is not a risk factor for obstetric complication: a historical cohort study. Harefuah 154(3):159–161
Raquil B, Joan Emilio L, Maria V, Carlos G, García G, de Casasola A, Zapatero, (2006) Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med 17:322–324
Cram P, Hillis SL, Barnett M, Rosenthal GE (2004) Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med 117:151–157
Bell CM, Redelmeier DA (2001) Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 345:663–668
Schilling PL, Campbell DA, Englesbe MJ, Davis MM (2010) A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care 48:224–232
Bailit JL, Landon MB, Thom E (2006) The MFMU Cesarean Registry: impact of time of day on cesarean complications. Am J Obstet Gynecol 195:1132–1137
Caughey AB, Urato AC, Lee KA (2008) Time of delivery and neonatal morbidity and mortality. Am J Obstet Gynecol 199(496):e1–5
Kalogiannidis I, MargioulaSiarkou C, Petousis S (2011) Infant births during the internal night are at increased risk for operative delivery and NICU admission. Arch Gynecol Obstet 284:65–71
American College of Obstetricians and Gynecologists (College) (2014) Society for maternal-fetal medicine, Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 210:179–193
American College of Obstetricians and Gynecologists (2014) Society for Maternal-Fetal Medicine. Safe prevention of the primary cesarean delivery. Obstetric care consensus no. 1. Obstet Gynecol 123:693–711
Committee on Practice Bulletins-Obstetrics (2017) Practice Bulletin No. 183: Postpartum Hemorrhage. Obstet Gynecol 130(4):e168–e186
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH (1994) Does housestaff discontinuity of care increase the risk for preventable adverse events? [comment]. Ann Intern Med 121:866–872
Peled Y, Melamed N, Chen R (2011) The effect of time of day on outcome of unplanned cesarean deliveries. J Matern Fetal Neonatal Med 24:1051–1054
Wu YW, Pham TN, Danielsen B, Towner D (2011) Nighttime delivery and risk of neonatal encephalopathy. Am J Obstet Gynecol 204(37):e1–6 (Epub 2010 Nov 11)
Funding
The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
EK: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing; SS: Data analysis; JA: Manuscript writing/editing; IW: Data analysis; IB: Data collection or management; EL: Data analysis; RG: Manuscript writing/editing; DV: Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The study was approved by the local research committee. Because the data set contained no patient identification information and all women received standard care, the study was exempt from informed consent requirements.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kadour-Peero, E., Sagi, S., Awad, J. et al. The impact of nurses’ and physicians’ shift change on obstetrical outcomes. Arch Gynecol Obstet 303, 653–658 (2021). https://doi.org/10.1007/s00404-020-05773-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05773-2