Abstract
Background
The ability of the pretreatment lymphocyte to monocyte ratio (LMR) to predict outcomes of patients with hepatocellular carcinoma (HCC) receiving sorafenib is not conclusively determined.
Methods
We retrospectively studied patients treated with sorafenib for HCC in two tertiary referral centres in Asia and North America. Primary endpoints were overall survival (OS) and progression-free survival (PFS). Predictive factors for the outcomes were determined by Cox proportional hazards models. A risk assessment tool was developed.
Results
Compared to the North America cohort, the Asia cohort was more heavily pretreated (72.1% vs. 35.2%; p < 0.001), had higher hepatitis B virus infection (87.6% vs. 5.6%; p < 0.001), and more distant metastases (83.2% vs. 25.4%; p < 0.001). Lower monocyte count in the Asia cohort (median 462.7 vs. 600.0/μL; p = 0.023) resulted in a higher LMR (median 2.6 vs. 1.8; p < 0.001). High LMR was associated with a significantly higher OS [hazard ratio (HR) 0.88; 95% confidence interval (CI) 0.81‒0.97; p = 0.007]. This was confirmed in a sensitivity analysis including patients treated in Asia only (HR 0.89; 95% CI 0.81‒0.97; p = 0.010). An OS nomogram was constructed with the following variables selected in the multivariate Cox model: LMR, treatment location, previous treatment, performance status, alpha-fetoprotein, lymph node metastasis, and Child‒Pugh score. The concordance score was 0.71 (95% CI, 0.67‒0.75). LMR did not predict PFS.
Conclusion
LMR measured before sorafenib administration predicts OS in advanced HCC patients. Our OS nomogram, incorporating LMR, can be offered to clinicians to improve their ability to assess prognosis, strengthen the prognosis-based decision-making, and inform patients in the clinic.


Similar content being viewed by others
Abbreviations
- LMR:
-
Lymphocyte to monocyte ratio
- TAM:
-
Tumor-associated macrophages
- HCC:
-
Hepatocellular carcinoma
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- SD:
-
Standard deviation
- IQR:
-
Interquartile ranges
- HR:
-
Hazard ratio
- HBV:
-
Hepatitis B virus
- ECOG:
-
Eastern Cooperative Oncology Group
- PT:
-
Prothrombin time
- AFP:
-
Alpha-fetoprotein
- TIL:
-
Tumor-infiltrating lymphocytes
- ALT:
-
Alanine aminotransferase
- HCV:
-
Hepatitis C virus
References
Dirkx AE, Oude Egbrink MG, Wagstaff J, Griffioen AW. Monocyte/macrophage infiltration in tumors: modulators of angiogenesis. J Leukoc Biol 2006;80(6):1183–1196. https://doi.org/10.1189/jlb.0905495(Epub 2006/09/26, PubMed PMID: 16997855)
Ribatti D, Nico B, Crivellato E, Vacca A. Macrophages and tumor angiogenesis. Leukemia 2007;21(10):2085–2089. https://doi.org/10.1038/sj.leu.2404900(Epub 2007/09/20, PubMed PMID: 17878921)
Roca H, Varsos ZS, Sud S, Craig MJ, Ying C, Pienta KJ. CCL2 and interleukin-6 promote survival of human CD11b+ peripheral blood mononuclear cells and induce M2-type macrophage polarization. J Biol Chem 2009;284(49):34342–34544. https://doi.org/10.1074/jbc.M109.042671(Epub 2009/10/17, PubMed PMID: 19833726; PubMed Central PMCID: PMCPMC2797202)
Song W, Tian C, Wang K, Zhang R-J, Zou S-B. The pretreatment lymphocyte to monocyte ratio predicts clinical outcome for patients with hepatocellular carcinoma: a meta-analysis. Sci Rep 2017;7:46601
Lin ZX, Ruan DY, Li Y, Wu DH, Ma XK, Chen J, et al. Lymphocyte-to-monocyte ratio predicts survival of patients with hepatocellular carcinoma after curative resection. World J Gastroenterol 2015;21(38):10898–10906. https://doi.org/10.3748/wjg.v21.i38.10898(Epub 2015/10/20, PubMed PMID: 26478681; PubMed Central PMCID: PMCPMC4600591)
Wu SJ, Lin YX, Ye H, Li FY, Xiong XZ, Cheng NS. Lymphocyte to monocyte ratio and prognostic nutritional index predict survival outcomes of hepatitis B virus-associated hepatocellular carcinoma patients after curative hepatectomy. J Surg Oncol 2016;114(2):202–210. https://doi.org/10.1002/jso.24297(Epub 2016/05/21, PubMed PMID: 27199001)
Cabrera R, Ararat M, Xu Y, Brusko T, Wasserfall C, Atkinson MA, et al. Immune modulation of effector CD4+ and regulatory T cell function by sorafenib in patients with hepatocellular carcinoma. Cancer Immunol Immunother 2013;62(4):737–746. https://doi.org/10.1007/s00262-012-1380-8(Epub 2012/12/12, PubMed PMID: 23223899; PubMed Central PMCID: PMCPMC3863727)
Bruix J, Cheng AL, Meinhardt G, Nakajima K, De Sanctis Y, Llovet J. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies. J Hepatol 2017;67(5):999–1008. https://doi.org/10.1016/j.jhep.2017.06.026(Epub 2017/07/09, PubMed PMID: 28687477)
Hipp MM, Hilf N, Walter S, Werth D, Brauer KM, Radsak MP, et al. Sorafenib, but not sunitinib, affects function of dendritic cells and induction of primary immune responses. Blood 2008;111(12):5610–5620
Chen Y, Huang Y, Reiberger T, Duyverman AM, Huang P, Samuel R, et al. Differential effects of sorafenib on liver versus tumor fibrosis mediated by stromal-derived factor 1 alpha/C-X-C receptor type 4 axis and myeloid differentiation antigen-positive myeloid cell infiltration in mice. Hepatology 2014;59(4):1435–1447. https://doi.org/10.1002/hep.26790(Epub 2013/11/19, PubMed PMID: 24242874; PubMed Central PMCID: PMCPMC3966948)
Flecken T, Schmidt N, Hild S, Gostick E, Drognitz O, Zeiser R, et al. Immunodominance and functional alterations of tumor-associated antigen-specific CD8+ T-cell responses in hepatocellular carcinoma. Hepatology 2014;59(4):1415–1426. https://doi.org/10.1002/hep.26731(Epub 2013/09/05, PubMed PMID: 24002931; PubMed Central PMCID: PMCPMC4139003)
Rosenberg SA. Progress in human tumour immunology and immunotherapy. Nature 2001;411(6835):380–384. https://doi.org/10.1038/35077246(Epub 2001/05/18, PubMed PMID: 11357146)
Malek E, de Lima M, Letterio JJ, Kim BG, Finke JH, Driscoll JJ, et al. Myeloid-derived suppressor cells: the green light for myeloma immune escape. Blood Rev 2016;30(5):341–348. https://doi.org/10.1016/j.blre.2016.04.002(Epub 2016/05/02, PubMed PMID: 27132116; PubMed Central PMCID: PMCPMC6411302)
Kuang DM, Zhao Q, Peng C, Xu J, Zhang JP, Wu C, et al. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med 2009;206(6):1327–1337. https://doi.org/10.1084/jem.20082173(Epub 2009/05/20, PubMed PMID: 19451266; PubMed Central PMCID: PMCPMC2715058)
Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 2004;4(1):71–78. https://doi.org/10.1038/nrc1256(Epub 2004/01/07, PubMed PMID: 14708027)
Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell 2006;124(2):263–266. https://doi.org/10.1016/j.cell.2006.01.007(Epub 2006/01/28, PubMed PMID: 16439202)
Steidl C, Lee T, Shah SP, Farinha P, Han G, Nayar T, et al. Tumor-associated macrophages and survival in classic Hodgkin’s lymphoma. N Engl J Med 2010;362(10):875–885. https://doi.org/10.1056/NEJMoa0905680(Epub 2010/03/12, PubMed PMID: 20220182; PubMed Central PMCID: PMCPMC2897174)
Mano Y, Yoshizumi T, Yugawa K, Ohira M, Motomura T, Toshima T, et al. Lymphocyte-to-monocyte ratio is a predictor of survival after liver transplantation for hepatocellular carcinoma. Liver Transpl 2018;24(11):1603–1611. https://doi.org/10.1002/lt.25204(Epub 2018/06/13, PubMed PMID: 29893464)
Lin B, Chen C, Qian Y, Feng J. Prognostic role of peripheral blood lymphocyte/monocyte ratio at diagnosis in diffuse large B-cell lymphoma: a meta-analysis. Leuk Lymphoma 2015;56(9):2563–2568. https://doi.org/10.3109/10428194.2015.1014367(Epub 2015/02/18, PubMed PMID: 25686648)
Porrata LF, Ristow K, Colgan JP, Habermann TM, Witzig TE, Inwards DJ, et al. Peripheral blood lymphocyte/monocyte ratio at diagnosis and survival in classical Hodgkin’s lymphoma. Haematologica 2012;97(2):262–269. https://doi.org/10.3324/haematol.2011.050138(Epub 2011/10/14, PubMed PMID: 21993683; PubMed Central PMCID: PMCPMC3269488)
Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev 2015;41(10):971–978. https://doi.org/10.1016/j.ctrv.2015.10.003(Epub 2015/10/21, PubMed PMID: 26481060)
Mao Y, Chen D, Duan S, Zhao Y, Wu C, Zhu F, et al. Prognostic impact of pretreatment lymphocyte-to-monocyte ratio in advanced epithelial cancers: a meta-analysis. Cancer Cell Int 2018;18:201. https://doi.org/10.1186/s12935-018-0698-5(Epub 2018/12/12, PubMed PMID: 30534002; PubMed Central PM CID: PMCPMC6282251)
Yang YT, Jiang JH, Yang HJ, Wu ZJ, Xiao ZM, Xiang BD. The lymphocyte-to-monocyte ratio is a superior predictor of overall survival compared to established biomarkers in HCC patients undergoing liver resection. Sci Rep 2018;8(1):2535. https://doi.org/10.1038/s41598-018-20199-2(Epub 2018/02/09, PubMed PMID: 29416061; PubMed Central PMCID: PMCPMC5803218)
Li GJ, Ji JJ, Yang F, Xu HW, Bai Y. Preoperative lymphocyte-to-monocyte ratio predicts survival in primary hepatitis B virus-positive hepatocellular carcinoma after curative resection. Onco Targets Ther 2017;10:1181–1189. https://doi.org/10.2147/ott.s110411(Epub 2017/03/07, PubMed PMID: 28260933; PubMed Central PMCID: PMCPMC5328305)
Zhu Z, Xu L, Zhuang L, Ning Z, Zhang C, Yan X, et al. Role of monocyte-to-lymphocyte ratio in predicting sorafenib response in patients with advanced hepatocellular carcinoma. Onco Targets Ther 2018;11:6731–6740. https://doi.org/10.2147/ott.s173275(Epub 2018/10/24, PubMed PMID: 30349306; PubMed Central PMCID: PMCPMC6188073)
Appel S, Rupf A, Weck MM, Schoor O, Brummendorf TH, Weinschenk T, et al. Effects of imatinib on monocyte-derived dendritic cells are mediated by inhibition of nuclear factor-kappaB and Akt signaling pathways. Clin Cancer Res 2005;11(5):1928–1940. https://doi.org/10.1158/1078-0432.Ccr-04-1713(Epub 2005/03/10, PubMed PMID: 15756019)
Borg C, Terme M, Taieb J, Menard C, Flament C, Robert C, et al. Novel mode of action of c-kit tyrosine kinase inhibitors leading to NK cell-dependent antitumor effects. J Clin Investig 2004;114(3):379–388. https://doi.org/10.1172/jci21102(Epub 2004/08/03, PubMed PMID: 15286804; PubMed Central PMCID: PMCPMC489961)
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 2009;10(1):25–34. https://doi.org/10.1016/s1470-2045(08)70285-7(Epub 2008/12/20., PubMed PMID: 19095497)
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359(4):378–390. https://doi.org/10.1056/NEJMoa0708857(Epub 2008/07/25, PubMed PMID: 18650514)
Sohn W, Paik YH, Cho JY, Lim HY, Ahn JM, Sinn DH, et al. Sorafenib therapy for hepatocellular carcinoma with extrahepatic spread: treatment outcome and prognostic factors. J Hepatol 2015;62(5):1112–1121. https://doi.org/10.1016/j.jhep.2014.12.009(Epub 2014/12/17, PubMed PMID: 25514557)
Cho JY, Paik YH, Lim HY, Kim YG, Lim HK, Min YW, et al. Clinical parameters predictive of outcomes in sorafenib-treated patients with advanced hepatocellular carcinoma. Liver Int 2013;33(6):950–957. https://doi.org/10.1111/liv.12168(Epub 2013/04/23, PubMed PMID: 23601249)
Geschwind JF, Kudo M, Marrero JA, Venook AP, Chen XP, Bronowicki JP, et al. TACE treatment in patients with sorafenib-treated unresectable hepatocellular carcinoma in clinical practice: final analysis of GIDEON. Radiology 2016;279(2):630–640. https://doi.org/10.1148/radiol.2015150667(Epub 2016/01/09, PubMed PMID: 26744927)
Abdel-Rahman O. Impact of baseline characteristics on outcomes of advanced HCC patients treated with sorafenib: a secondary analysis of a phase III study. J Cancer Res Clin Oncol 2018;144(5):901–908. https://doi.org/10.1007/s00432-018-2610-z(Epub 2018/02/20, PubMed PMID: 29455421)
Ghany MG, Morgan TR. Hepatitis C guidance 2019 update: American Association for the study of liver diseases-infectious diseases Society of America recommendations for testing, managing, and treating hepatitis c virus infection. Hepatology 2020;71(2):686–721. https://doi.org/10.1002/hep.31060(Epub 2019/12/10, PubMed PMID: 31816111)
Kwon BS, Jeong DH, Byun JM, Lee TH, Choi KU, Song YJ, et al. Prognostic value of preoperative lymphocyte-monocyte ratio in patients with ovarian clear cell carcinoma. J Cancer 2018;9(7):1127–1134. https://doi.org/10.7150/jca.24057(Epub 2018/04/21, PubMed PMID: 29675093; PubMed Central PMCID: PMCPMC5907660)
Ma JY, Liu Q. Clinicopathological and prognostic significance of lymphocyte to monocyte ratio in patients with gastric cancer: a meta-analysis. Int J Surg 2018;50:67–71. https://doi.org/10.1016/j.ijsu.2018.01.002(Epub 2018/01/14, PubMed PMID: 29329786)
Zhu X, Wu SQ, Xu R, Wang YH, Zhong ZH, Zhang L, et al. The evaluation of monocyte lymphocyte ratio as a preoperative predictor in urothelial malignancies: a pooled analysis based on comparative studies. Sci Rep 2019;9(1):6280. https://doi.org/10.1038/s41598-019-42781-y(Epub 2019/04/20, PubMed PMID: 31000754; PubMed Central PMCID: PMCPMC6472363)
Yang JD, Mohamed EA, Aziz AO, Shousha HI, Hashem MB, Nabeel MM, et al. Characteristics, management, and outcomes of patients with hepatocellular carcinoma in Africa: a multicountry observational study from the Africa Liver Cancer Consortium. Lancet Gastroenterol Hepatol 2017;2(2):103–111. https://doi.org/10.1016/s2468-1253(16)30161-3(Epub 2017/04/14, PubMed PMID: 28403980)
Funding
National Institutes of Health to LRR (R01 CA 186566), the Mayo Clinic Hepatobiliary SPORE (P50 CA 210964), the Mayo Clinic Cancer Center (P30 CA 15083), the Mayo Clinic Center for Clinical and Translational Science (UL1 TR 002377).
Author information
Authors and Affiliations
Contributions
YH—conceptualisation, data curation, investigation, and wiring—original draft; MAMA—conceptualisation, data curation, and writing—original draft; MMP—formal analysis, methodology, and writing—review and editing; WSH—formal analysis, methodology, and writing—review and editing; TMT—formal analysis, methodology, and writing—review and editing; HCL—writing—review and editing, BYR—writing—review and editing; SB—data curation; KAV—data curation; MM—data curation; VRM—data curation; KP—data curation.
Corresponding authors
Ethics declarations
Conflict of interest
Dr. Lewis Roberts has received grant support from ARIAD Pharmaceuticals, Bayer, BTG International, Exact Sciences, Gilead Sciences, Glycotest Inc., RedHill Inc., Target PharmaSolutions, and Wako Diagnostics; he has provided advisory services to Bayer, Exact Sciences, Gilead Sciences, GRAIL Inc., QED Therapeutics and TAVEC. The other authors have no conflicts of interests to declare.
Informed consent in human subjects
The institutional review board of the Asan Medical Center (approval number: 2019-0685) and the Mayo Clinic (approval number: 15-006298) granted a waiver of informed consent and approval of this observational study with deidentified data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12072_2020_10076_MOESM1_ESM.tif
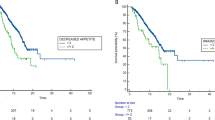
Supplemental Digital Content 1 Kaplan–Meier estimate of overall survival in the entire cohort. CI, Confidence Interval (TIF 72 kb)
12072_2020_10076_MOESM2_ESM.tif
Supplemental Digital Content 2 Kaplan–Meier estimate of progression-free survival in the entire cohort. CI, Confidence Interval (TIF 70 kb)
Rights and permissions
About this article
Cite this article
Ha, Y., Mohamed Ali, M.A., Petersen, M.M. et al. Lymphocyte to monocyte ratio-based nomogram for predicting outcomes of hepatocellular carcinoma treated with sorafenib. Hepatol Int 14, 776–787 (2020). https://doi.org/10.1007/s12072-020-10076-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10076-4