Abstract
Background and Objective
Breast cancer is the second leading cause of cancer death worldwide. The economic burden of breast cancer is crucial for the sustainability of healthcare systems. The objective of this study was to estimate the burden of HR+/HER2− metastatic breast cancer (MBC) in Italy, in terms of incidence, prescription patterns, healthcare resource utilisation and costs for the National Health System (NHS).
Methods
A cohort study based on healthcare administrative data (ReS database), covering > 10 million Italians, was performed. Incident cases of HR+/HER2− MBC were identified among adult women in 2013. The cohort was followed-up for 2 years to describe healthcare utilisation and integrated costs (pharmaceuticals, hospitalisations and outpatient services) for NHS. Prescription patterns were described as first-line choice and therapeutic changes. Specific therapeutic changes were used as proxies of disease progression. A survival analysis was performed to estimate the time from diagnosis to first disease progression.
Results
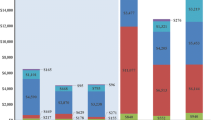
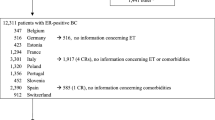
Of 5174,723 women, 355 cases of de novo HR+/HER2− MBC were selected (incidence: 6.9 per 100,000). During the 1st follow-up year, they generated an average cost of €7543, whereas €4834 in the 2nd year. The 85.9% received a monotherapy, while the 14.1% received a combination therapy. The most used monotherapy was nonsteroidal-aromatase-inhibitors (45.9%), while the most prescribed combination was tamoxifen + luteinizing hormone releasing hormone (LHRH) analogues (6.2%). Therapeutic changes occurred in 45.4% of patients, especially from chemotherapy to nonsteroidal-aromatase-inhibitors, after an average of 276.8 days from the first treatment. Disease progression was identified in 22.5% of patients occurring after a mean 13 ± 6 months from diagnosis.
Conclusions
This detailed picture of HR+/HER2− MBC, based on real-world data, could be helpful in health technology assessment and expenditure forecasts of future therapeutic strategies for this condition in Italy.

Similar content being viewed by others
References
International Agency for Research on Cancer (IARC). Cancer fact sheets: Breast, Source: Globocan 2018. https://gco.iarc.fr/today/data/factsheets/cancers/20-Breast-fact-sheet.pdf. Accessed 24 July 2019.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
van ‘t Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AA, Mao M, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415(6871):530–6.
van de Vijver MJ, He YD, van ‘t Veer LJ, Dai H, Hart AA, Voskuil DW, et al. A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347(25):1999–2009.
Rivenbark AG, O’Connor SM, Coleman WB. Molecular and cellular heterogeneity in breast cancer: challenges for personalized medicine. Am J Pathol. 2013;183(4):1113–24.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14(12):1165–74.
Parisi M, Pelletier C, Cherepanov D, Broder MS. Outcomes research examining treatments, quality of life and costs in HER2− negative and triple-negative metastatic breast cancer: a systematic literature review. J Comp Eff Res. 2018;7(1):67–83.
Piccinni C, Ronconi G, Calabria S, Dondi L, Forcesi E, Rossi E, et al. Healthcare resources utilisation in primary progressive multiple sclerosis. Neurol Sci. 2018;39(7):1169–74.
Calabria S, Forcesi E, Dondi L, Pedrini A, Maggioni AP, Martini N. Target population of non-deferrable surgery and uncontrolled severe bleeding related to dabigatran. Cardiovasc Drugs Ther. 2018;32(3):281–6.
Schifano P, Papini P, Agabiti N, Scarinci M, Borgia P, Perucci CA. Indicators of breast cancer severity and appropriateness of surgery based on hospital administrative data in the Lazio Region, Italy. BMC Public Health. 2006;6:25.
Nordstrom BL, Whyte JL, Stolar M, Mercaldi C, Kallich JD. Identification of metastatic cancer in claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 2):21–8.
Kahn LH, Blustein J, Arons RR, Yee R, Shea S. The validity of hospital administrative data in monitoring variations in breast cancer surgery. Am J Public Health. 1996;86(2):243–5.
Hao Y, Li N, Fang AP, Koo V, Peeples M, Kageleiry A, et al. Real-world analysis of medical costs and healthcare resource utilization in elderly women with HR+/HER2− metastatic breast cancer receiving everolimus-based therapy or chemotherapy. Adv Ther. 2016;33(6):983–97.
Vaz-Luis I, Lin NU, Keating NL, Barry WT, Lii H, Winer EP, et al. Racial differences in outcomes for patients with metastatic breast cancer by disease subtype. Breast Cancer Res Treat. 2015;151(3):697–707.
Jacquet E, Lardy-Cleaud A, Pistilli B, Franck S, Cottu P, Delaloge S, et al. Endocrine therapy or chemotherapy as first-line therapy in hormone receptor-positive HER2− negative metastatic breast cancer patients. Eur J Cancer (Oxford, England: 1990). 2018;95:93–101.
Ciruelos E, Perez-Garcia JM, Gavila J, Rodriguez A, de la Haba-Rodriguez J. Maintenance therapy in HER2− negative metastatic breast cancer: a new approach for an old concept. Clin Drug Investig. 2019;39(7):595–606.
Crocetti E, Gori S, Falcini F. Metastatic breast cancers: Estimates for Italy. Tumori. 2018;104(2):116–20.
Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M. Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol Biomark Prev. 2017;26(6):809–15.
Bertaut A, Mounier M, Desmoulins I, Guiu S, Beltjens F, Darut-Jouve A, et al. Stage IV breast cancer: a population-based study about prognostic factors according to HER2 and HR status. Eur J Cancer Care. 2015;24(6):920–8.
Tao L, Chu L, Wang LI, Moy L, Brammer M, Song C, et al. Occurrence and outcome of de novo metastatic breast cancer by subtype in a large, diverse population. Cancer Causes Control. 2016;27(9):1127–38.
Gobbini E, Ezzalfani M, Dieras V, Bachelot T, Brain E, Debled M, et al. Time trends of overall survival among metastatic breast cancer patients in the real-life ESME cohort. Eur J Cancer (Oxford, England: 1990). 2018;96:17–24.
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Ribociclib as first-line therapy for HR-Positive, advanced breast cancer. N Engl J Med. 2016;375(18):1738–48.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2− negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–39.
Capri S, Russo A. Cost of breast cancer based on real-world data: a cancer registry study in Italy. BMC Health Serv Res. 2017;17(1):84.
Pawaskar M, Karve S, Dalvi T, Davis KL, Deeter R, editors. Health care utilization and costs among HER2− negative, HR-positive, elderly women with metastatic breast cancer in the United States. In: 2013 ASCO annual meeting; 2013 31 May–4 June 2013; Chicago, IL, USA.
van Walraven C, Austin P. Administrative database research has unique characteristics that can risk biased results. J Clin Epidemiol. 2012;65(2):126–31.
Gini R, Schuemie MJ, Pasqua A, Carlini E, Profili F, Cricelli I, et al. Monitoring compliance with standards of care for chronic diseases using healthcare administrative databases in Italy: strengths and limitations. PLoS One. 2017;12(12):e0188377.
Broekx S, Den Hond E, Torfs R, Remacle A, Mertens R, D’Hooghe T, et al. The costs of breast cancer prior to and following diagnosis. Eur J Health Econ. 2011;12(4):311–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the study.
Conflict of interest
CP, LD, GR, SC, AP, IE, NM and MM declare that they have no conflict of interest.
Ethical approval
This is an observational, non-interventional database study, re-utilising administrative data, primary collected for governance purposes. The study was conducted under specific agreements between Fondazione ReS and Italian Regional/Local Health Facilities, participating with anonymous data to the ReS database. All these institutions have general legal and ethical frameworks that allow them for conducting analyses, aimed to address governance and research questions, by making secondary use of anonymous administrative data.
Informed consent
No informed consent is required to use anonymous patient data which is analysed retrospectively.
Additional information
Part of results of this study has been submitted as abstracts to the Italian Society of Pharmacology 39th annual national meeting (20–23 November 2019, Firenze) and to AIOM (Italian Association of Medical Oncology) 21st annual national meeting (25–27 October 2019, Roma).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Piccinni, C., Dondi, L., Ronconi, G. et al. HR+/HER2− Metastatic Breast Cancer: Epidemiology, Prescription Patterns, Healthcare Resource Utilisation and Costs from a Large Italian Real-World Database. Clin Drug Investig 39, 945–951 (2019). https://doi.org/10.1007/s40261-019-00822-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-019-00822-4