Abstract
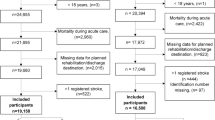
The aim of this study was to assess the association between admission to stroke centers for acute ischemic stroke and complications and mortality during hospitalization in a Chinese population by means of an observational study using data from the China Stroke Center Data-Sharing Platform. We compared in-hospital complications and mortality for patients admitted with acute ischemic stroke (N = 13,236) between November 1, 2018 and December 31, 2018 at stroke center (SH) and non-stroke center (CH) hospitals using distance to hospitals as an instrumental variable to adjust for potential prehospital selection bias. The results showed that complication rates during hospitalization among ischemic stroke patients who received thrombolytic therapy (n = 11,203) were lower in the SH group than in the CH group: 11.1% vs 15.7% (absolute difference, − 5.11% [95% CI, − 6.05 to − 3.99%], odds ratio [OR] 0.85 [95% CI, 0.74 to 0.92]). The incidence of intracranial hemorrhage was reduced from 4.2 to 3.2%: SH group vs CH group, 3.2% vs 4.2% (absolute difference, − 1.24% [95% CI, − 1.65 to − 0.82%], OR 0.83 [95% CI, 0.69 to 0.0.98]). Furthermore, the total mortality rate in the SH group was also lower than in the CH group: SH group vs CH group, 2.2% vs 3.0% (absolute difference, − 0.92% [95% CI, − 1.48 to − 0.53%], OR 0.85 [95% CI, 0.73 to 0.96]). The data showed that admission to SH hospitals was associated with a lower risk of treatment complications and death for patients with an acute ischemic stroke receiving thrombolytic therapy.


Similar content being viewed by others
Data Availability
Please contact the correspondence author for the data request.
References
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135:759–71.
The GBD 2016 Lifetime Risk of Stroke Collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379:2429–37.
Lu H, Guo Z, Liu J, et al. Trends in stroke incidence among elderly low-income residents of rural China: a population-based study from 1992 to 2016. Aging (Albany NY). 2018;10(11):3438–49.
Wang Z, Hu S, Sang S, Luo L, Yu C. Age-period-cohort analysis of stroke mortality in China: data from the Global Burden of Disease Study 2013. Stroke. 2017;48:271–5.
Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405 6. https://www.jointcommission.org/assets/1/6/TJC-Stroke-brochure-vfinal-low-rez1.PDF.
Waje-Andreassen U, Nabavi DG, Engelter ST, Dippel DWJ, Jenkinson D, Skoda O, et al. European stroke organisation certification of stroke units and stroke centres. Eur Stroke J. 2018;3:220–6.
Lichtman JH, Jones SB, Leifheit-Limson EC, Wang Y, Goldstein LB. 30-day mortality and readmission after hemorrhagic stroke among Medicare beneficiaries in Joint Commission primary stroke center-certified and noncertified hospitals. Stroke. 2011;42(12):3387–91.
Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305(4):373–80.
Guan T, Ma J, Li M, Xue T, Lan Z, Guo J, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology. 2017;89:53–61.
Longde W, Ling Y, Yang H, Yi Z, Yongjun W, Xunming J, et al. Fixed-dose combination treatment after stroke for secondary prevention in China: a national community-based study. Stroke. 2015;46:1295–300.
Wang Y, Li Z, Zhao X, Wang C, Wang X, Wang D, et al. Effect of a multifaceted quality improvement intervention on hospital personnel adherence to performance measures in patients with acute ischemic stroke in China: a randomized clinical trial. JAMA. 2018;320(3):245–54.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–34.
Warlow CP, Sudlow C, Dennis M, Wardlaw J, Sandercock P. Stroke. Lancet. 2003;362:1211–24.
Man S, Cox M, Patel P, Smith EE, Reeves MJ, Saver JL, et al. Differences in acute ischemic stroke quality of care and outcomes by primary Stroke Center Certification Organization. Stroke. 2017;48(2):412–9.
Meretoja A, Roine RO, Kaste M, Linna M, Roine S, Juntunen M, et al. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: a nationwide observational study from Finland. Stroke. 2010;41(6):1102–7.
Rudd AG, Hoffman A, Irwin P, Lowe D, Pearson MG. Stroke unit care and outcome: results from the 2001 National Sentinel Audit of Stroke (England, Wales, and Northern Ireland). Stroke. 2005;36(1):103–6.
Jarman B, Aylin P, Bottle A. Acute stroke units and early CT scans are linked to lower in-hospital mortality rates. BMJ. 2004;328:369.
Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651–65.
Paul Coverdell Prototype Registries Writing Group*. Acute stroke care in the US: results from 4 pilot prototypes of the Paul Coverdell National Acute Stroke Registry. Stroke. 2005;36(6):1232–40.
Reeves MJ, Broderick JP, Frankel M, LaBresh KA, Schwamm L, Moomaw CJ, et al. The Paul Coverdell National Acute Stroke Registry: initial results from four prototypes. Am J Prev Med. 2006;31(S2):S202–9.
Langhorne P, O’Donnell MJ, Chin SL, et al. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. Lancet. 2018;391:2019–27.
Li S, Cui LY, Anderson C, Zhu S, Xu P, Wei T, et al. Public awareness of stroke and the appropriate responses in China: a cross-sectional community-based study (FAST-RIGHT). Stroke. 2019;50(2):455–62.
Wang Y, Liao X, Zhao X, Wang DZ, Wang C, Nguyen-Huynh MN, et al. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese National Stroke Registry (CNSR). Stroke. 2011;42:1658–64.
Bouckaert M, Lemmens R, Thijs V. Reducing prehospital delay in acute stroke. Nat Rev Neurol. 2009;5:477–83.
Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–8.
Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke. 2008;39:3262–7.
Gladstone DJ, Rodan LH, Sahlas DJ, Lee L, Murray BJ, Ween JE, et al. A citywide prehospital protocol increases access to stroke thrombolysis in Toronto. Stroke. 2009;40:3841–4.
Tong D, Reeves MJ, Hernandez AF, Zhao X, Olson DWM, Fonarow GC, et al. Times from symptom onset to hospital arrival in the Get with the Guidelines–Stroke program 2002 to 2009: temporal trends and implications. Stroke. 2012;43:1912–7.
Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012;43(2):362–70.
Walter S, Kostopoulos P, Haass A, Keller I, Lesmeister M, Schlechtriemen T, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol. 2012;11:397–404.
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke. Circulation. 2007;115:e478–534.
Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue plasminogen activator in the treatment of acute stroke: the Standard Treatment With Alteplase to Reverse Stroke (STARS) Study. JAMA. 2000;283:1145–50.
Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke–Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275–82.
Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology. 2000;55:1649–55.
Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–15.
LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med. 2008;168:411–7.
California Acute Stroke Pilot Registry (CASPR) Investigators. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005;64:654–9.
Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007;297(3):278–85.
Acknowledgements
We thank Hugh McGonigle, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of the manuscript. We especially want to express our gratitude to those doctors and medical staff who participated in the clinical data collection. We need special thanks Dr. Gang Xu (The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China), Dr. Yang Yang (Hengshui Harrison International Peace Hospital, Hengshui, China) and Mr. Xiao-Dong Niu (China Stroke Data Center, Beijing, China) who had helped us to collect data and perform statistical processing.
Participating Hospitals
Capital Medical University Xuanwu Hospital; Tianjin Huanhu Hospital; Shanghai Changhai Hospital; Chuzhou Central Hospital; Hebei Medical University Second Hospital; General Hospital of the Northern War Zone of the Chinese People’s Liberation Army; Dalian Central Hospital; Shenyang First People’s Hospital; Jilin University First Hospital; Jilin City Center Hospital; Jiangsu Provincial People’s Hospital; Nanjing Gulou Hospital; Nanjing First Hospital; The First Affiliated Hospital of Suzhou University; Second Affiliated Hospital of Zhejiang University School of Medicine; Henan Provincial People’s Hospital; First Affiliated Hospital of Zhengzhou University; West China Hospital of Sichuan University; Liaocheng People’s Hospital, Xi’an Jiaotong University First Affiliated Hospital; Anhui Provincial Hospital; Zhengzhou Central Hospital; Wuhan First Hospital; Zhoukou Central Hospital; Guizhou Medical University Affiliated Hospital; Linyi People’s Hospital; Nanyang Central Hospital; Hubei Provincial Third People’s Hospital; Harbin Medical University Affiliated Second Hospital; Yichang Central People’s Hospital;
Peking University Third Hospital; More hospitals information can be found at https://www.sinosc.org/WebManage/StrokeCenter/StrokeCenter
Funding
This study was supported by grants from National Health and Family Planning Commission of China.
Author information
Authors and Affiliations
Contributions
Wang LD had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Tu WJ, Shen Y, Chao BH, Cao L, and Wang LD contributed to the study concept and design. Tu WJ, Chao BH, and Shen Y contributed to the acquisition of the data. Tu WJ, Chao BH, and Cao L carried out the analysis and interpretation of the data. Tu WJ, Shen Y, Chao BH, and Cao L contributed in the drafting of the manuscript. Wang LD is responsible for the critical revision of the manuscript for important intellectual content. Tu WJ, Shen Y, and Chao BH are responsible for the administrative, technical, or material support. Wang LD obtained the funding. Wang LD supervised.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
This study was approved by the institutional review board of Capital Medical University Xuanwu Hospital, with waiver for informed consent.
Role of the Sponsor
The funding organizations had no role in the design and concept of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 139 kb)
Rights and permissions
About this article
Cite this article
Shen, Y., Chao, BH., Cao, L. et al. Stroke Center Care and Outcome: Results from the CSPPC Stroke Program. Transl. Stroke Res. 11, 377–386 (2020). https://doi.org/10.1007/s12975-019-00727-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-019-00727-6