Abstract
Purpose of Review
A considerable body of data from genetic and epidemiological studies strongly support a causal relationship between high lipoprotein(a) [Lp(a)] levels, and the development of atherosclerosis and cardiovascular disease. This relationship is continuous, unrelated to Lp(a) threshold, and independent of low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol levels. Unfortunately, the mechanism(s) through which Lp(a) promotes atherosclerosis are not clarified yet. Suggested hypotheses include: an increased Lp(a)-associated cholesterol entrapment in the arterial intima followed by inflammatory cell recruitment, abnormal upload of proinflammatory oxidized phospholipids, impaired fibrinolysis by inhibition of plasminogen activation, and enhanced coagulation, through inhibition of the tissue factor pathway inhibitor. This review is aimed at summarizing the available evidence on the topic.
Recent Findings
There are two clinical forms, isolated hyperlipidemia(a) [HyperLp(a)] with acceptable LDL-C levels (< 70 mg/dL), and combined elevation of Lp(a) and LDL-C in plasma. To date, no drugs that selectively decrease Lp(a) are available. Some novel lipid-lowering drugs can lower Lp(a) levels, but to a limited extent, as their main effect is aimed at decreasing LDL-C levels. Significant Lp(a) lowering effects were obtained with nicotinic acid at high doses. However, adverse effects apart, nicotinic acid is no longer prescribed and available in Europe for clinical use, after European Agency of Medicines (EMA) ban.
Summary
The only effective therapeutic option for now is Lipoprotein Apheresis (LA), albeit with some limitations. Lastly, it is to be acknowledged that the body of evidence confirming that reducing plasma isolated elevation of Lp(a) brings cardiovascular benefit is still insufficient. However, the growing bulk of clinical, genetic, mechanistic, and epidemiological available evidence strongly suggests that Lp(a) is likely to be the smoking gun.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kiechl S, Willeit J. The mysteries of lipoprotein(a) and cardiovascular disease revisited. J Am Coll Cardiol. 2010;55(19):2168–70.
Page MM, Stefanutti C, Sniderman A, Watts GF. Recent advances in the understanding and care of familial hypercholesterolaemia: significance of the biology and therapeutic regulation of proprotein convertase subtilisin/kexin type 9. Clin Sci (Lond). 2015;129(1):63–79.
Tsimikas S, Witztum JL. The role of oxidized phospholipids in mediating lipoprotein(a) atherogenicity. Curr Opin Lipidol. 2008;19:369–77.
Hervio L, Chapman MJ, Thillet J, Loyau S, Anglés-Cano E. Does apolipoprotein(a) heterogeneity influence lipoprotein(a) effects on fibrinolysis? Blood. 1993;82:392–7.
Danesh J, Collins R, Peto R. Lipoprotein(a) and coronary heart disease. Meta-analysis of prospective studies. Circulation. 2000;102:1082–5.
Dahlen G, Ericson C, Furberg C, Lundkvist L, Sveardsudd K. Studies on an extra pre-beta lipoprotein fraction. Acta Med Scand. 1972;531(Suppl):1–29.
Bennet A, Di Angelantonio E, Erqou S, Eiriksdottir G, Sigurdsson G, et al. Lipoprotein(a) levels and risk of future coronary heart disease: large-scale prospective data. Arch Intern Med. 2008;168:598–608.
Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, et al. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–23.
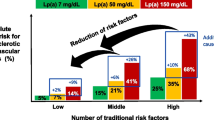
•• Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG. Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease. N Engl J Med. 2016;375(24):2349–58 This study shows that both genetic and lifestyle factors contribute to individual-level risk of coronary artery disease. The study is worth for the large number of patients observed.
Erqou S, Thompson A, Di Angelantonio E, Saleheen D, Kaptoge S, et al. Apolipoprotein(a) isoforms and the risk of vascular disease: systematic review of 40 studies involving 58,000 participants. J Am Coll Cardiol. 2010;55:2160–7.
Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009;301:2331–9.
Virani SS, Brautbar A, Davis BC, Nambi V, Hoogeveen RC, Sharrett AR, et al. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2012;125:241–9.
Geethanjali FS, Luthra K, Lingenhel A, Kanagasaba-Pathy AS, Jacob J, et al. Analysis of the apo(a) size polymorphism in Asian Indian populations: association with Lp(a) concentration and coronary heart disease. Atherosclerosis. 2003;169:121–30.
McPherson R, Pertsemlidis A, Kavaslar N, Stewart A, Roberts R, Cox DR, et al. A common allele on chromosome 9 associated with coronary heart disease. Science. 2007;316(5830):1488–91.
Akaike M, Azuma H, Kagawa A, Matsumoto K, Hayashi I, et al. Effect of aspirin treatment on serum concentrations of lipoprotein(a) in patients with atherosclerotic diseases. Clin Chem. 2002;48:1454–9.
Gaeta G, Lanero S, Barra S, Silvestri N, Cuomo V, Materazzi C, et al. Sex hormones and lipoprotein(a) concentration. Expert OpinInvestig Drugs. 2011;20:221–2238.
Jaeger BR, Richter Y, Nagel D, Heigl F, Vogt A, Roeseler E, et al. Longitudinal cohort study on the effectiveness of lipid apheresis treatment to reduce high lipoprotein(a) levels and prevent major adverse coronary events. Nat Clin Pract Cardiovasc Med. 2009;6:229–39.
Merki E, Graham M, Taleb A, Leibundgut G, Yang X, Miller ER, et al. Antisense oligonucleotide lowers plasma levels of apolipoprotein (a) and lipoprotein (a) in transgenic mice. J Am Coll Cardiol. 2011;57:1611–21.
Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol. 2013;62(23):2178–84.
Cuchel M, Bloedon LT, Szapary PO, Kolansky DM, Wolfe ML, et al. Inhibition of microsomal triglyceride transfer protein in familial hypercholesterolemia. N Engl J Med. 2007;356(2):148–56.
Cuchel M, Meagher EA, du Toit TH, Blom DJ, Marais AD, et al. Phase 3 HoFHLomitapide Study investigators. Efficacy and safety of a microsomal triglyceride transfer protein inhibitor in patients with homozygous familial hypercholesterolaemia: a single-arm, open-label, phase 3 study. Lancet. 2013;381(9860):40–6.
Desai NR, Kohli P, Giugliano RP, O’Donoghue ML, Somaratne R, et al. AMG145, a monoclonal antibody against proprotein convertase subtilisinkexin type 9, significantly reduces lipoprotein(a) in hypercholesterolemic patients receiving statin therapy: an analysis from the LDL-C Assessment with Proprotein Convertase SubtilisinKexin Type 9 Monoclonal Antibody Inhibition Combined with Statin Therapy (LAPLACE)-Thrombolysis in Myocardial Infarction (TIMI) 57 trial. Circulation. 2013;128(9):962–9.
Gotto AM Jr, Cannon CP, Li XS, Vaidya S, Kher U, et al. Evaluation of lipids, drug concentration, and safety parameters following cessation of treatment with the cholesteryl ester transfer protein inhibitor anacetrapib in patients with or at high risk for coronary heart disease. Am J Cardiol. 2013;113(1):76–83.
Gouni-Berthold I, Berthold HK. Lipoprotein(a): current perspectives. Curr Vasc Pharmacol. 2011;9:682–92.
Sahebkar A, Simental-Mendía LE, Stefanutti C, Pirro M. Supplementation with coenzyme Q10 reduces plasma lipoprotein(a) concentrations but not other lipid indices: a systematic review and meta-analysis. Pharmacol Res. 2016;105:198–209.
Viney NJ, van Capelleveen JC, Geary RS, Xia S, Tami JA, Yu RZ, et al. Antisense oligonucleotides targeting apolipoprotein(a) in people with raised lipoprotein(a): two randomised, double-blind, placebo-controlled, dose-ranging trials. Lancet. 2016;388(10057):2239–53.
Hovland A, Marcovina S, Hardersen R, Enebakk T, Mollnes TE, et al. Three different LDL apheresis columns efficiently and equally reduce lipoprotein(a) concentrations in patients with familial hypercholesterolemia and small apolipoprotein(a) particles. Transfus Apher Sci. 2012;46:73–6.
Kassner U, Schlabs T, Rosada A, Steinhagen-Thiessen E. Lipoprotein(a) - an independent causal risk factor for cardiovascular disease and current therapeutic options. Atheroscler Suppl. 2015;18:263–7.
Schettler V, Neumann CL, Hulpke-Wette M, Hagenah GC, Schulz EG, et al. Current view: indications for extracorporeal lipid apheresis treatment. Clin Res Cardiol Suppl. 2012;7:15–9.
Derfler K, Steiner S, Sinzinger H. Lipoprotein-apheresis: Austrian consensus on indication and performance of treatment. Wien KlinWochenschr. 2015;127:655–63.
Stefanutti C. The 2009 2nd Italian Consensus Conference on LDL-apheresis. Nutr Metab Cardiovasc Dis. 2010;20:761–2.
Stefanutti C, D’Alessandri G, Russi G, De Silvestro G, Zenti MG, et al. Treatment of symptomatic hyperLp(a)lipoproteinemia with LDL-apheresis: a multicentre study. Atheroscler Suppl. 2009;10:89–94.
Kronenberg F, Utermann G. Lipoprotein(a): resurrected by genetics. J Intern Med. 2013;273:6–30.
• Roeseler E, Julius U, Heigl F, Spitthoever R, Heutling D, et al. Lipoprotein apheresis for lipoprotein(a)-associated cardiovascular disease: prospective 5 years of follow-up and apolipoprotein(a) characterization. Arterioscler Thromb Vasc Biol. 2016;36:2019–27 This study confirmed that after 5 years of prospective follow-up LA has a lasting effect on prevention of cardiovascular events in patients with HyperLp(a).
Stefanutti C, Vivenzio A, Di Giacomo S, Mazzarella B, Ferraro PM, et al. Treatment of symptomatic hyperLp(a)lipidemia with LDL-apheresis vs. usual care. Transfus Apher Sci. 2010;42:21–6.
Leebmann J, Roeseler E, Julius U, Heigl F, Spitthoever R, Heutling D, et al. Lipoprotein apheresis in patients with maximally tolerated lipid-lowering therapy, lipoprotein(a)-hyperlipoproteinemia, and progressive cardiovascular disease: prospective observational multicenter study. Circulation. 2013;128:2567–76.
Rosada A, Kassner U, Vogt A, Willhauck M, Parhofer K, Steinhagen-Thiessen E. Does regular lipid apheresis in patients with isolated elevated lipoprotein(a) levels reduce the incidence of cardiovascular events? Artif Organs. 2014;38:135–41.
Safarova MS, Ezhov M, Afanasieva O, Matchin YG, Atanesyan RV, et al. Effect of specific lipoprotein(a) apheresis on coronary atherosclerosis regression assessed by quantitative coronary angiography. Atheroscler Suppl. 2013;14:93–9.
von Dryander M, Fischer S, Passauer J, Müller G, Bornstein SR, Julius U. Differences in the atherogenic risk of patients treated by lipoprotein apheresis according to their lipid pattern. Atheroscler Suppl. 2013;14:39–44.
Stefanutti C, Morozzi C. HyperLp(a)lipoproteinaemia: unmet need of diagnosis and treatment? Blood Transfus. 2016;14(5):408–12.
•• Schatz U, Tselmin S, Müller G, Julius U, Hohenstein B, et al. Most significant reduction of cardiovascular events in patients undergoing lipoprotein apheresis due to raised Lp(a) levels—a multicenter observational study. Atheroscler Suppl. 2017;30:246–52 This study reported that during long-term treatment with LA, a significant reduction of CV events/patient in all vessel beds was confirmed.
Stefanutti C, Thompson GR. Lipoprotein apheresis in the management of familial hypercholesterolaemia: historical perspective and recent advances. Curr Atheroscler Rep. 2015;17(1):465.
Stefanutti C, Julius U, Watts GF, Harada-Shiba M, Cossu M, Schettler VJ, et al. Toward an international consensus-integrating lipoprotein apheresis and new lipid-lowering drugs. J Clin Lipidol. 2017;11(4):858–71.
Lippi G, Franchini M, Targher G. Screening and therapeutic management of lipoprotein(a) excess: review of the epidemiological evidence, guidelines and recommendations. Clin Chim Acta. 2011;412(11–12):797–801.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Thomas M. Stulnig, Claudia Morozzi, Roman Reindl-Schwaighofer, and Claudia Stefanutti declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Evidence-Based Medicine
Glossary
- Kringle
-
protein structure characterized by an amino acid chain wrapped in fashion to remember a Danish pastry called “Kringle.” This conformation is maintained from three intra-catenary disulfide bridges present in fixed positions of the sequence primary amino acid.
- SNP
-
Single-nucleotide polymorphism.
Rights and permissions
About this article
Cite this article
Stulnig, T.M., Morozzi, C., Reindl-Schwaighofer, R. et al. Looking at Lp(a) and Related Cardiovascular Risk: from Scientific Evidence and Clinical Practice. Curr Atheroscler Rep 21, 37 (2019). https://doi.org/10.1007/s11883-019-0803-9
Published:
DOI: https://doi.org/10.1007/s11883-019-0803-9