Abstract
Lupus anticoagulants (LA) are a heterogeneous group of antiphospholipid antibodies (aPLAs) that promote thrombosis. Tissue factor (TF)–bearing extracellular vesicles (EVs) might contribute to the prothrombotic state of patients with persistent LA and a history of thrombosis. To investigate if EV-associated TF activity is elevated in a well-defined group of LA-positive patients with a history of thrombosis in comparison to that of healthy controls. Adult patients (n = 94, median age 40.1 years, interquartile range (IQR) 29.9–53.4; 87% females) positive for LA and a history of thrombosis (78% venous thrombosis, 17% arterial thrombosis, 5% venous thrombosis and arterial thrombosis) and healthy age- and sex-matched controls (n = 30, median age 42.9 years, IQR 38.6–45.8, 77% females) were included in this study. EV-TF activity was determined with a factor Xa generation assay and anti-β2-glycoprotein (anti-β2GPI) and anticardiolipin (aCL) antibodies by enzyme-linked immunoassays. EV-TF activity did not differ between 94 LA-positive patients with a history of thrombosis (median 0.05 pg/mL, IQR 0.00–0.14) and 30 healthy controls (median 0.06, IQR 0.00–0.11, p = 0.7745). No correlation was found between EV-TF activity and lupus-sensitive activated partial thromboplastin time (aPTT-LA) (rho = 0.034), Rosner index (rho = − 0.056), anti-β2GPI IgG (rho = 0.05), anti-β2GPI IgM (rho = − 0.08), aCL IgG (rho = 0.12), and aCL IgM (rho = − 0.11) in LA-positive patients. We found low EV-TF activity levels in LA-positive patients and a history of thrombosis and no correlation with analyzed aPLAs. Our data indicate that circulating TF-bearing EVs do not contribute to the prothrombotic state of patients with LA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
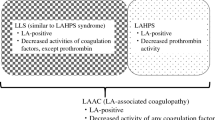
The term lupus anticoagulant (LA) was coined to describe the phenomenon of plasma samples from patients with systemic lupus erythematosus (SLE) that fail to clot within the appropriate time [1]. First regarded as a laboratory curiosity, it turned out that LA are a heterogeneous class of prothrombotic immunoglobulins that either directly or indirectly target phospholipids [2]. Persistently elevated LA, anticardiolipin (aCL), and/or anti-ß2 glycoprotein (anti-β2GPI) antibodies together with a history of thrombotic events or pregnancy complications define the antiphospholipid syndrome (APS) [3, 4].
Tissue factor (TF) is a transmembrane glycoprotein and the main initiator of the blood coagulation cascade [5]. Active TF is absent from the circulation under physiologic conditions [6], but antiphospholipid antibodies induce the expression of TF on peripheral blood mononuclear cells [7, 8]. Elevated levels of TF-exposing extracellular vesicles (EVs) were found in APS patients in studies that applied flow cytometry [9, 10]. However, the validity of such studies has been questioned due to a lack of reproducibility and detection of encrypted functionally inactive TF [11,12,13,14]. Functional EV-associated TF activity assays are more reliable for the quantification of procoagulant TF in plasma than antigen assays [14]. In a recent study, levels of EV-TF activity were measured in patients with APS and increased EV-TF activity was found in APS patients compared to asymptomatic individuals with elevated antiphospholipid antibodies [15].
In the present study, we measured EV-TF activity in 94 patients with LA and a history of thrombosis and in 30 matched healthy controls with a well-established functional EV-TF activity assay [14] to determine if TF-exposing EVs contribute to the prothrombotic state of APS.
Patients and methods
Ninety-four adult APS patients with persistently positive LA (confirmed 12 weeks apart) [4] and a history of thrombosis were included and were recruited between May 2001 and 2014. All registered events had to be symptomatic and the thrombotic event had to be diagnosed with standardized methods as described [16]. A blood sample was drawn at study inclusion.
The ethics committee of the Medical University of Vienna in accordance with the Declaration of Helsinki approved the conduct of the study (EC no. 068/2001 and 1268/2014), and each patient provided written informed consent.
Blood sampling and sample preparation
Blood was collected with a 21-gauge butterfly needle (Greiner Bio-One, Kremsmünster, Austria) into a VACUETTE tube (Greiner Bio-One, Kremsmünster, Austria) containing one-tenth volume sodium citrate stock solution at 0.129 mM by atraumatic and sterile antecubital venipuncture. Platelet-poor plasma was prepared by centrifugation at 2500g for 15 min at 15 °C, aliquoted, and stored at − 80 °C until measurements were performed in series.
EV-TF activity assay
EV-associated TF activity measurements were performed as previously described [17].
Determination of LA
LA was diagnosed according to the recommendations of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis [18, 19] and as described [16]. Two different screening tests including a lupus-sensitive activated partial thromboplastin time (PTT-LA, Diagnostica Stago, Asnières-sur-Seine, France) and a diluted Russell viper venom time were used for LA determination. For patients who received vitamin K antagonists (VKAs) as anticoagulation, only aPTT was used for screening. As soon as one or both screening tests were prolonged, further analysis and confirmatory tests were performed on these samples, as described elsewhere [20].
Patients, whose LA confirmatory tests were not clearly positive but had a Rosner index (calculated as 100 × (clotting times of the 1:1 mixture − normal plasma)/patient’s plasma) value above 15, were still considered LA positive [21]. The StaClot LA (Diagnostica Stago, Asnières-sur-Seine, France) and the dRVVT-LA confirm (Life Diagnostics, Clarkston, GA, USA) were used as confirmatory assay.
Determination of aCL and anti-β2GPI antibodies
Indirect solid-phase enzyme immunoassays were used to detect immunoglobulin G (IgG) and IgM antibodies against β2GPI and aCL. The Varelisa Cardiolipin test (Pharmacia (Phadia AB), Uppsala, Sweden) was used to detect antibodies semiautomatically using a Tecan Genesis liquid handling system (Tecan Group Ltd., Männedorf, Switzerland) between 2001 and September 2005. Afterwards, the Orgentec Cardiolipin and starting from October 2006, the Orgentec β2GPI tests (both from Orgentec, Mainz, Germany) were used on a fully automated BEP2000 Advance System (Siemens Healthcare Diagnostics, Marburg, Germany) as standard routine assays. All assays were performed following the manufacturers’ instructions. Results were reported positive, if a titer > 99th percentile for anti-β2GPI and aCL IgG and/or IgM antibodies was detected, according to the Sydney Consensus Statement on Investigational Classification Criteria for the Antiphospholipid Antibody Syndrome [4].
Statistics
Continuous variables were described by the median and the interquartile range (IQR) indicating the 25th–75th percentile. Categorical variables were described by the absolute numbers and percentages. Wilcoxon-Mann-Whitney U test was used to analyze differences between two groups, and Kruskal-Wallis test was used for comparison of more than two groups. The correlation between variables was assessed by Spearman’s rank correlation coefficient. Two-sided p values smaller than 0.05 were considered statistically significant. Statistical analysis was performed using SPSS version 17.0.2 (SPSS Inc., Chicago, USA), and graphs were done with GraphPad Prism 6 (GraphPad Software, Inc., San Diego, CA, USA).
Results
Patient characteristics
Ninety-four LA-positive patients (87% female) with a history of thrombosis (78% venous thrombosis, 17% arterial thrombosis, 5% venous thrombosis and arterial thrombosis) were included in this study. Out of these 94 patients, 22 (23.4%) were tested for LA alone, 8 (8.5%) for LA + aCL antibodies, and 64 (68.1%) were positively tested for LA, anti-β2GPI, and aCL antibodies (triple positive).
At study inclusion, 83 (88.3%) patients were taking oral anticoagulation (OAC), 9 patients (9.6%) were taking low-dose aspirin, 67 (71.1%) patients were taking VKAs, 7 (7.4%) were taking low-dose aspirin and VKAs, and 11 (11.7%) patients received no anticoagulant therapy. Additionally 30 age- and sex-matched patients without a history of thrombosis were included in this study.
Table 1 summarizes the baseline demographic, clinical, and laboratory data of patients and controls.
EV-TF activity in lupus anticoagulant–positive patients with a history of thrombosis and healthy controls
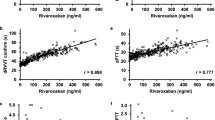
The coefficient of variation of the EV-TF activity assay was calculated to analyze the reproducibility of the assay. Within this study, the intra-assay variability was 20% and the inter-assay variability was 22%, which is within the range of other studies [17, 22]. The median EV-TF activity was 0.05 pg/mL (IQR 0.00–0.14) in the LA-postive patients compared to 0.06 pg/mL (IQR 0.00–0.11) in 30 healthy individuals. No significant difference in EV-TF activity was found between these two groups (Wilcoxon-Mann-Whitney U test: p = 0.7745, Fig. 1). Moreover, no difference in EV-TF activity was found between patients that had a history of venous thrombosis or arterial thrombosis or both before inclusion into the study (Kruskal-Wallis test for differences between groups: p = 0.545, Fig. 2). Results from this study showed no difference in EV-TF activity between patients positive for LA alone, patients positive for LA in combination with aCL, or triple positive patients (Kruskal-Wallis test for differences between groups: p = 0.5304, Fig. 3) Furthermore, EV-TF activity did neither differ between patients taking OAC and patients without anticoagulant therapy (Wilcoxon-Mann-Whitney U test: p = 0.9602, Fig. 4) nor between patients taking LDA, VKA, or both in combination (Kruskal-Wallis test for differences between groups: p = 0.8098, Fig. 5). Analysis of EV-TF activity between patients with one, two, or more thromboembolic events showed no statistical difference (Kruskal-Wallis test for differences between groups: p = 0.449, Fig. 6).
Although analysis of the influence of storage time on EV-TF activity levels has to be interpreted with caution, as most measurements were below the detection limit, it was possible to perform a linear regression analysis. In this analysis, we observed an R2 value of 0.021, suggesting that storage time only explained 2.1% in the variability of EV-TF levels.
In a raw data analysis of generated FXa (indicating EV-TF activity [pg/mL]), a normal distribution around zero was found in APS patients indicating that no EV-TF activity above the background of the assay was detectable in these patients (Fig. 7).
Correlations between EV-TF activity, lupus anticoagulant, and antiphospholipid antibodies in patients with antiphospholipid syndrome
No correlation was found between EV-TF activity and aPTT-LA (rho = 0.034), Rosner index (rho = − 0.056), anti-β2GPI IgG (rho = 0.05), anti-β2GPI IgM (rho = − 0.08), aCL IgG (rho = 0.12), and aCL IgM (rho = − 0.11) in LA-positive patients with a history of thrombosis.
Discussion
In this study, we measured plasma EV-TF activity in a well-defined group of LA-positive patients with a history of thrombosis and in a group of age- and sex-matched healthy individuals. EV-TF activity did not differ between LA-positive patients and healthy individuals. Furthermore, no differences in EV-TF activity could be detected within the LA-positive group, analyzed for type of thrombosis, antibody positivity, or OAC. Raw data analysis of FXa generation measurements (indicating EV-TF activity) in LA-positive patients showed a normal distribution of around zero indicating that EV-TF activity was not detectable. Therefore, data from our study do not show that circulating TF-exposing EVs are elevated and that they contribute to the development of thrombosis in LA-positive patients.
Willemze et al. also determined EV-TF activity in APS patients with an assay that is comparable to ours [15]. Consistent with our present results, they found low EV-TF activity in APS patients (median 0.13 pg/mL [IQR 0.10–0.17]), but EV-TF activity was significantly higher than in asymptomatic individuals with positive antiphospholipid antibodies (median 0.09 pg/mL [IQR 0.05–0.14]). Consistent with our study, they found no differences in subgroup analyses of APS patients. Interestingly, EV-TF activity of healthy individuals was higher in a previous publication by this group [23] than EV-TF activity of APS patients in the aforementioned study [15].
The EV-TF activity assay used in our study is the, to date, most widely applied and best described assay for the quantification of TF-exposing EVs in clinical samples. Hisada et al. report on the application of this assay in 32 clinical trials and the sensitivity for the detection of TF-exposing EVs in different prothrombotic conditions [14]. Moreover, Hisada et al. found that plasma preparation affects EV-TF activity levels. They found a significantly lower EV-TF activity in platelet-free plasma from healthy controls than in platelet-poor plasma [14]. In our present study and the study by Willemze et al. centrifugation of plasma samples differed, which could be an explanation for different results. It is a limitation of our study that no additional functional assays were applied for the quantification procoagulant EVs. For example, modified thrombin generation assays [24, 25] or prothrombinase assays [26, 27] would have added valuable additional information about the procoagulant properties of EVs in our study population. However, patient material was very limited, and therefore, we could not perform additional measurements.
Data from experimental studies indicate that a “second prothrombotic hit” might be needed for the development of APS, because in mouse models, elevated antiphospholipid antibodies promoted thrombosis only in presence of vascular damage, endothelial activation, or inflammation [28, 29]. Consistent with this notion, during the observation period of our patients, smoking and diabetes were strong risk factors for developing thrombosis, which therefore represent two potential factors of the aforementioned “second hit phenomenon” [30]. Data from our study do not indicate that TF-bearing EVs contribute to this “second hit.” However, we cannot exclude a role of very low levels of TF-bearing EVs, which cannot be detected with our assay [22].
The lack of EV-TF activity in our present study does not exclude a role for monocyte-bound TF in the prothrombotic state of APS patients. Zhou et al. found that monocyte-associated TF activity was increased by anti-ß2GPI autoantibodies from APS patients [31]. Similar results were obtained by Kornberg et al. and by Reverter et al. who used in vitro generated aCL antibodies [32, 33]. Surprisingly, no study was published so far that directly found elevated TF activity on monocytes from APS patients.
In conclusion, data from this study do not support the assumption that TF-exposing EVs play an important role in the prothrombotic state of persistently LA-positive patients with a history of thrombosis.
References
Feinstein DI, Rapaport SI (1972) Acquired inhibitors of blood coagulation. Prog Hemost Thromb 1:75–95
Tripodi A (2007) Laboratory testing for lupus anticoagulants: a review of issues affecting results. Clin Chem 53:1629–1635
Giannakopoulos B, Krilis SA (2013) The pathogenesis of the antiphospholipid syndrome. N Engl J Med 368:1033–1044
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost : JTH. 4:295–306
Spronk HM, Govers-Riemslag JW, ten Cate H (2003) The blood coagulation system as a molecular machine. BioEssays 25:1220–1228
Butenas S, Mann KG (2004) Active tissue factor in blood? Nat Med 10:1155–1156 author reply 6
Butenas S, Bouchard BA, Brummel-Ziedins KE, Parhami-Seren B, Mann KG (2005) Tissue factor activity in whole blood. Blood 105:2764–2770
Amengual O, Atsumi T, Khamashta MA, Hughes GR (1998) The role of the tissue factor pathway in the hypercoagulable state in patients with the antiphospholipid syndrome. Thromb Haemost 79:276–281
Vikerfors A, Mobarrez F, Bremme K, Holmstrom M, Agren A, Eelde A et al (2012) Studies of microparticles in patients with the antiphospholipid syndrome (APS). Lupus 21:802–805
Chaturvedi S, Cockrell E, Espinola R, Hsi L, Fulton S, Khan M, Li L, Fonseca F, Kundu S, McCrae KR (2015) Circulating microparticles in patients with antiphospholipid antibodies: characterization and associations. Thromb Res 135:102–108
Lacroix R, Robert S, Poncelet P, Kasthuri RS, Key NS, Dignat-George F et al (2010) Standardization of platelet-derived microparticle enumeration by flow cytometry with calibrated beads: results of the International Society on Thrombosis and Haemostasis SSC Collaborative workshop. J Thromb Haemost 8:2571–2574
Lacroix R, Judicone C, Poncelet P, Robert S, Arnaud L, Sampol J et al (2012) Impact of pre-analytical parameters on the measurement of circulating microparticles: towards standardization of protocol. J Thromb Haemost 10:437–446
Coumans FAW, Brisson AR, Buzas EI, Dignat-George F, Drees EEE, El-Andaloussi S et al (2017) Methodological guidelines to study extracellular vesicles. Circ Res 120:1632–1648
Hisada Y, Alexander W, Kasthuri R, Voorhees P, Mobarrez F, Taylor A, McNamara C, Wallen H, Witkowski M, Key NS, Rauch U, Mackman N (2016) Measurement of microparticle tissue factor activity in clinical samples: a summary of two tissue factor-dependent FXa generation assays. Thromb Res 139:90–97
Willemze R, Bradford RL, Mooberry MJ, Roubey RA, Key NS (2014) Plasma microparticle tissue factor activity in patients with antiphospholipid antibodies with and without clinical complications. Thromb Res 133:187–189
Gebhart J, Posch F, Koder S, Perkmann T, Quehenberger P, Zoghlami C, Ay C, Pabinger I (2015) Increased mortality in patients with the lupus anticoagulant: the Vienna Lupus Anticoagulant and Thrombosis Study (LATS). Blood 125:3477–3483
Khorana AA, Francis CW, Menzies KE, Wang JG, Hyrien O, Hathcock J et al (2008) Plasma tissue factor may be predictive of venous thromboembolism in pancreatic cancer. J Thromb Haemost : JTH. 6:1983–1985
Brandt JT, Triplett DA, Alving B, Scharrer I (1995) Criteria for the diagnosis of lupus anticoagulants: an update. On behalf of the Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the ISTH. Thromb Haemost 74:1185–1190
Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M et al (2009) Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost : JTH. 7:1737–1740
Wenzel C, Stoiser B, Locker GJ, Laczika K, Quehenberger P, Kapiotis S, Frass M, Pabinger I, Knöbl P (2002) Frequent development of lupus anticoagulants in critically ill patients treated under intensive care conditions. Crit Care Med 30:763–770
Rosner E, Pauzner R, Lusky A, Modan M, Many A (1987) Detection and quantitative evaluation of lupus circulating anticoagulant activity. Thromb Haemost 57:144–147
Lee RD, Barcel DA, Williams JC, Wang JG, Boles JC, Manly DA, Key NS, Mackman N (2012) Pre-analytical and analytical variables affecting the measurement of plasma-derived microparticle tissue factor activity. Thromb Res 129:80–85
Stravitz RT, Bowling R, Bradford RL, Key NS, Glover S, Thacker LR, Gabriel DA (2013) Role of procoagulant microparticles in mediating complications and outcome of acute liver injury/acute liver failure. Hepatology 58:304–313
Hellum M, Franco-Lie I, Ovstebo R, Hauge T, Henriksson CE (2017) The effect of corn trypsin inhibitor, anti-tissue factor pathway inhibitor antibodies and phospholipids on microvesicle-associated thrombin generation in patients with pancreatic cancer and healthy controls. PLoS One 12:e0184579
Gheldof D, Haguet H, Dogne JM, Bouvy C, Graux C, George F et al (2017) Procoagulant activity of extracellular vesicles as a potential biomarker for risk of thrombosis and DIC in patients with acute leukaemia. J Thromb Thrombolysis 43:224–232
Thaler J, Ay C, Weinstabl H, Dunkler D, Simanek R, Vormittag R, Freyssinet JM, Zielinski C, Pabinger I (2011) Circulating procoagulant microparticles in cancer patients. Ann Hematol 90:447–453
Jy W, Horstman LL, Jimenez JJ, Ahn YS, Biro E, Nieuwland R et al (2004) Measuring circulating cell-derived microparticles. J Thromb Haemost : JTH 2:1842–1851
Fischetti F, Durigutto P, Pellis V, Debeus A, Macor P, Bulla R et al (2005) Thrombus formation induced by antibodies to beta2-glycoprotein I is complement dependent and requires a priming factor. Blood 106:2340–2346
Arad A, Proulle V, Furie RA, Furie BC, Furie B. beta(2)-Glycoprotein-1 autoantibodies from patients with antiphospholipid syndrome are sufficient to potentiate arterial thrombus formation in a mouse model. Blood 2011;117:3453–3459
Posch F, Gebhart J, Rand JH, Koder S, Quehenberger P, Pengo V, Ay C, Pabinger I (2017) Cardiovascular risk factors are major determinants of thrombotic risk in patients with the lupus anticoagulant. BMC Med 15:54
Zhou H, Wolberg AS, Roubey RA (2004) Characterization of monocyte tissue factor activity induced by IgG antiphospholipid antibodies and inhibition by dilazep. Blood 104:2353–2358
Kornberg A, Blank M, Kaufman S, Shoenfeld Y (1994) Induction of tissue factor-like activity in monocytes by anti-cardiolipin antibodies. J Immunol 153:1328–1332
Reverter JC, Tassies D, Font J, Khamashta MA, Ichikawa K, Cervera R et al (1998) Effects of human monoclonal anticardiolipin antibodies on platelet function and on tissue factor expression on monocytes. Arthritis Rheum 41:1420–1427
Funding
Open access funding provided by Austrian Science Fund (FWF). This work was supported by the Austrian Science Fund (FWF), Special Research Program (SFB) 5405-B21 and 5404-B21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The ethics committee of the Medical University of Vienna in accordance with the Declaration of Helsinki approved the conduct of the study (EC no. 068/2001 and 1268/2014) and each patient provided written informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hell, L., Ay, C., Posch, F. et al. Low extracellular vesicle–associated tissue factor activity in patients with persistent lupus anticoagulant and a history of thrombosis. Ann Hematol 98, 313–319 (2019). https://doi.org/10.1007/s00277-018-3544-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3544-x